CancerSurvivorMD®
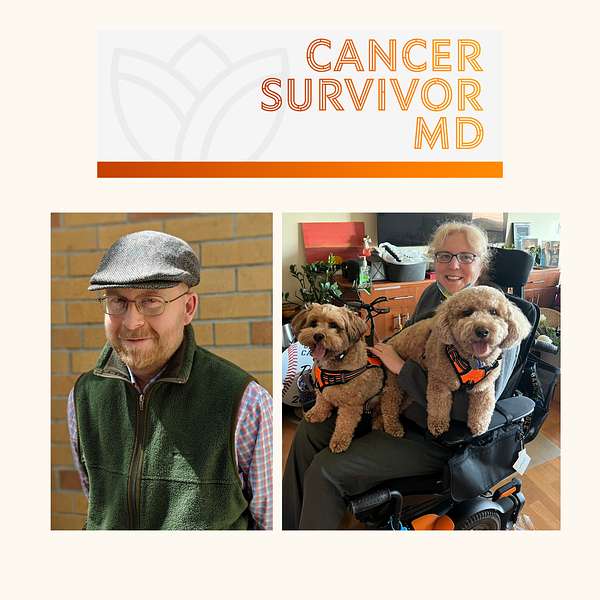
Hello! Welcome to CancerSurvivorMD’s podcast by Brad and Josie!
We will share our experiences with living in sickness, health, and anything in between to allow healing and growth. The topics will focus on cancer survivors and caregivers but will likely resonate with anyone who has been diagnosed with any health condition.
Brad is a retired English professor and cancer survivor, now a facilitator of the Writing as Healing workshop.
Josie is a retired medical oncologist and cancer survivor.
If you have any questions or topic suggestions, please send them our way, and we will try to incorporate your request.
Please take a look at the disclaimers (https://cancersurvivormd.org/disclaimers). Words can hurt—if you feel you might get or have been triggered, please stop listening and seek support.
CancerSurvivorMD®
Author Chat with Jill Squire, BSN, RN, OCN
Discover the essential tools and wisdom to empower yourself or a loved one through a cancer journey in our latest episode. Featuring author Jill Squire and her groundbreaking book "Cancer Journey Guide and Journals: Empowerment in Diagnosis and Treatment and Beyond," we explore practical strategies to support cancer patients from diagnosis through long-term survivorship.
This conversation promises invaluable insights into self-advocacy, effective communication, and the significance of tracking symptoms and treatments in a user-friendly format.
Engage in a heartening discussion on the power of self-care activities like birding and mindfulness, which are essential tools for managing symptoms and maintaining mental wellness. Learn how to build a robust cancer care team, navigate tough conversations with loved ones, and utilize guided journals to keep track of your journey. By sharing personal stories, practical advice, and compassionate guidance, our panel aims to empower you with the knowledge and confidence to take charge of your healthcare experience.
We also delve into the critical aspect of building trust with healthcare providers and the role of daily symptom tracking in shared decision-making. Jill Squire provides expert tips on creating useful diaries to document experiences, which can significantly enhance communication with healthcare professionals. Concluding on a light-hearted note with a pun to bring some humor, we express gratitude to Jill and reflect on the book's unique value for anyone facing a challenging diagnosis. Join us for this heartfelt and informative episode designed to uplift and empower.
Relevant links for Jill Squire, BSN, RN, OCN:
- Jill's first book.
- Jill's LinkedIn profile.
- Jill's podcast.
- Jill's facebook profile.
- Jill's Patreon profile.
- Jill's YouTube profile.
General Links:
- Disclaimers: https://cancersurvivormd.org/disclaimers/
- Brad Buchanan: https://linktr.ee/bradthechimera
- G [Josie] van Londen: https://linktr.ee/cancersurvivormd
- CancerBridges: https://cancerbridges.org/
Welcome again to our general weekly group. I am Wendy Myers, one of the senior clinical managers, social worker at Cancer Bridges. Tonight we're doing one of our book talks and I want to introduce two people instrumental in developing these book talks and actually was one of the authors. He's also a cancer survivor. He's joining us from the West Coast. We're excited to have Brad here. And then we have our lovely Dr Josie Van London, who many of you know. She is a physician as well as a cancer survivor an amazing wealth of knowledge. She has her own podcast. She has her own Instagram called Cancer Survivor MD. So Brad and Josie put their heads together, along with Jen and myself, and we created this book talk. Here we are and tonight we have one of our own who actually presented a couple months ago on this group although she's going to do a little different vibe on this her amazing new book. I'm going to let Jen introduce her. Everybody get comfortable. We'll have a chance for some questions later. Take it away, ms Jennifer.
Jen Kehm:Thank you, wendy. So I am Jen Kemp. I'm the Program and Development Coordinator at Cancer Bridges also a survivor. This is Jill's book, which I have known Jill for a long time. She is a facilitator at Cancer Bridges. I'll read you her bio because it's pretty amazing.
Jen Kehm:Jill Squire is a longtime registered nurse with over a decade of experience in oncology, nursing navigation and case management. She is a devoted cancer support group facilitator for Cancer Bridges and holds the members and leadership team in the highest regard as an avid content creator and podcast host and the well-received Everything Cancer podcast. Our executive director was interviewed and it was an excellent podcast with both of you. It's called Everything Cancer podcast. Jill is passionate about developing survivor-centric content, providing education and collaborating with professionals to improve survivorship care. She is committed to empowering survivors and guiding them toward efficient, effective and self-advocacy shared decision-making with their healthcare team.
Jen Kehm:Jill published this book, which is what we're talking about tonight Cancer Journey Guide and Journals Empowerment and Diagnosis and Treatment and Beyond in February 2024, with electronic versions set to be available on Amazon by the end of September. That's fantastic. She's also co-representing a webinar on shared decision-making through the National Coalition of Cancer Survivorship at the end of October. That's amazing. Jill is applying for grants this fall and hopes to be hearing more from her soon. I can't say enough about Jill. I have gone through the book and it's amazing. There's so much content that is so relevant whether you are newly diagnosed or out of treatment, but still trying to navigate through survivorship. So with that, I will turn you over to Jill and I'm going to unspotlight myself and Wendy so that everyone can discuss.
Jill Squire:I'm so honored to be here, jen, I feel like you're talking about someone else. Brad, I waved when Wendy said your, because I heard about you through Michelle Kirshner, who I'm getting to know very well. Josie, an honor to meet you.
G van Londen:Same here, jill, I'm very excited. I was going to repeat a little bit an overview of the book and ask you a few questions. Hopefully you will have Learned something new and feel empowered, which is always the goal of these sessions. This book my summary of it Is amazing.
G van Londen:It has a font that's readable. It's large, not too dense Word choice. It's very easy to read, even if you have brain fog. There are just enough words to know where to go and get more information and it touches on everything you need to know when you've been newly diagnosed with cancer and moving forward on your whole journey, including the long-term survivorship phase journey, including the long-term survivorship phase. It's empowering how it captures the various things that you can help yourself or knowing where to go if you need help beyond what you can do for yourself and how to formulate questions and what if you lock trust in your providers.
G van Londen:I think at least 75% of the book is for you to fill out. It contains empty forms that you can use to track your symptoms medications, doctors, appointments, what was discussed in the appointments. It goes on and on and all of it is super helpful. You can tear it out, leave it in the book and just take your book with you when you go to your appointments. The other thing that I thought was funny in the end there's two pages that are a collection of jokes and things that make you laugh and smile, which goes to say that humor plays a very important role in your coping mechanisms too. I will hand it over to Jill. Then.
G van Londen:I had two main questions to ask Jill. One is what made you write this book? What was the big driver? Because I don't think anybody else has created a book like this. This is very unique in how it has a very easy to grasp knowledge and information combined with a workbook that you can use to track everything in your life, health wise. It's not out there, as far as I know, not to this professional degree, written by a nurse. So what made you write this and who did you intend to write the book?
Jill Squire:for. Thank you so much, dr Van London, for that amazing introduction. And who did you intend to write the book for? Thank you so much, dr Van London, for that amazing introduction. This book is written for anybody facing a tough diagnosis.
Jill Squire:The reason why I wrote it and it is directed towards people dealing with cancer which is obvious by the content, but I think almost anybody can pick it up that's dealing with something that's tough and they need to advocate for themselves for the rest of their life and need to track their symptoms. That's a really tough thing to have to do, and not only are you having to advocate for yourself and formulate your thoughts for your healthcare team, but also with your family, because sometimes you find yourself at opposite ends of the spectrum and that can be a really tough place to be. They're not in your shoes. You need to learn how to be a good listener with them, but you also need to understand where you're coming from, formulate those thoughts, have a good outcome in those conversations and hopefully help them learn how to advocate for you. If not, then agree to disagree but ultimately end up with a supportive relationship. It's really hard when you don't.
Jill Squire:The reason I ultimately put this together and it was a four-year goal was as a navigator. I navigated for three years. I did gynecology for a year and a half and then it's actually almost four years. I was a lead navigator for two and a half years. I covered all the areas and worked with all the navigators there. I came across so many gaps in care that were inadvertent, but if someone had known how to advocate for themselves or understood their treatment plan better I'm not putting the onus on the patient at all, it doesn't belong there but maybe some of those gaps in care might have been avoided. But also shared decision making didn't happen where maybe it should have, and so that became really important to me. It's become much more prevalent, but it still isn't where it needs to be. It was born of that. That became very evident to me also as a case manager, and then facilitating the support group only supported that idea, and so I became very passionate about effective self-advocacy, empowerment and shared decision-making faces with a little question mark.
G van Londen:Not everybody here may understand the concept of shared decision-making. I wonder if you would be willing to expand a little bit on that. While it looks like you're pulling up something there, let me tell the group that Jill is a very kind soul. She is not in this field for profit. She's in this field, for empowerment, which makes the difference, we need people like Jill, but I think she understood that there needs to be more people than just Jill.
G van Londen:And one of the ways she can do that is by writing a book. Now I'm going to sidetrack a little bit, but the survivorship field as a whole is struggling with how to help all of you. There's different ways in which it's proposed that we can do this and different levels depending on how much support somebody needs. The lower level of support is self-help materials, and that is where this book fits in. Most of you don't need anything beyond that, but if you do, then that book hopefully will make you feel empowered enough to say, hey, you need to refer me on to a higher level of support so I can be helped.
G van Londen:And, jill, it sounds like you're working on other clinical resources to be more hands-on with individuals, because some do need a little bit more help. So shared decision-making to go back to where I left, jill is ensured the fact that a provider and a patient talk together and discuss the pros and cons of a particular medical intervention and together decide what is best for the patient. At the end of the day, though, it's the patient's decision, but it's an informed conversation that leads your patient to make a decision.
Jill Squire:I have a really good example of that from a few years ago. There was a patient who was very in tune with their job and their job was very important to them. They were on a maintenance treatment that their provider had recommended to them. They were finding it really hard to go to work and engage in work. It was the optimal treatment. And they sat down with their provider and said I can't make it to work every day on this treatment and I want it cut back in frequency. Their provider, their oncologist, replied I mean, this is really boiling it down. You will have a higher chance of recurrence if you have your treatment less frequently. And the patient's response was but my life isn't worth living not being able to do what I want to do and I want to be able to engage in my work because it has that much value to me and I want to spend time with my family, enjoying time with my family. And so they agreed together to decrease his treatment intervals. He now has three good weeks in between. He recovers well, he is fully engaged in work. He's fully engaged in life. He's going on vacations, knowing that his life may be shorter, but he is enjoying it much more. So that was a shared decision. It was an informed decision. But his point to his oncologist was that he was miserable the other way and that's a fairly stark example. It's an example that actually occurred.
Jill Squire:And another example I have is a patient who had a strong belief in faith for control of her symptoms and her oncologist was pretty insistent on anti-emetics.
Jill Squire:She said to her oncologist I don't want them, I want to use faith to try and control my symptoms for as long as I can. And her oncologist agreed that they would go for as long as they could and her oncologist would try and not give as much with the treatments. This patient probably did better than I've ever seen anybody do through really tough treatments without as much upfront anti medication. She eventually did say to her oncologist okay, I'm ready. But they communicated every single treatment about how she was doing and I wouldn't be one bit surprised if that oncologist ends up presenting that patient at a conference down the road. But it was a shared decision on what was important to that patient to try and the decision wasn't taken away from her by the oncologist saying this is our protocol that we follow. The oncologist explained to her that it's really important you stay hydrated. It's really important you're able to drink and you need to tell me when you're not able to anymore.
G van Londen:Yeah, I like that. There's so much in what you're saying that deserves its own discussion. I usually compare it to Eeyore and Tigger. We're all different Compared to Eeyore and Tigger. We're all different and we need to find a treatment or a medical decision that fits with who you are, how you stand in life. Some of you are like Tigger, like you want to deal with it now, bouncing up and down. Some of you might be more like Eeyore Well, I'll deal with it when it flies in my face, and maybe then I still won't deal with it. And so everybody makes their own decisions. We may not agree with your decision, but as long as you're cognitively intact, then we have to accept what you're deciding.
G van Londen:In a nutshell, this book is about you understanding that you have a voice you can voice about your questions, your complaints, no matter how minor they are compared to your life and death scenario. Even hot flashes overnight can be a big hinder on your quality of life, your sleeping, your ability to function during the day. So this book, I think, is about empowerment. But, jill, would you like to share your screen and maybe go through the table of contents to show people? And I think Brett you look like you had a question.
Brad Buchanan:I do have a question. I don't know if it's the right time for it, but I was just going to comment from a patient's perspective. I think your book would be really helpful, because people don't want to seem stupid, right? They don't want to seem like they're saying something dumb, and giving them the confidence to be a good advocate for themselves is really important if you want that shared decision-making that we're talking about. Right, and I guess what I'm getting at is having this journal. This workbook is a place for you to record all the details of each visit so that you are prepared for the next one and you can go in with the right tools in your toolbox, so to speak.
Brad Buchanan:I took about seven different chemo drugs at various points and couldn't always remember the names of each of them. They decided to change the regimen a little bit. Anyway, the long and the short of it is, I think patients really need to feel confident enough to be good self-advocates and to participate in shared decision-making, and your book seems like it's going to be an important tool for people in that regard. I salute you for that. My question was about the birthing nurse and whether that has any like. I think it's important to remember that your patients are full human beings with their disease, and I think it's really great that there are nurses and medical professionals with pursuits and passions outside of their profession. I wonder if that passion, that outlet that you have on social media plays a role somehow in your approach to medicine treatment, your career.
Jill Squire:I encourage people to make sure that they're able to do something they enjoy and I also bring that up in self-advocacy to outline what's important to you. Birding is important to me. It's my Zen place. Sometimes I have to remind myself to do something I enjoy. It's really easy getting too involved in the creative process and you need a break from it. I hope that answered your question. I'm going to share my screen and I just need a minute. Here we go. Can everybody see this now? This explains quickly how to use the journal. The first part is an outline of actual steps to advocating for yourself and being empowered, and the second part are the journals, which is a key part of being empowered. And here are the table of contents to the empowerment piece. These are the basics of effective self-advocacy, of effective self-advocacy and, as you can see, several of them can be listed on the same page.
Jill Squire:As Dr Van London pointed out, these are intended to be very short and easy to read. I intentionally stayed away from being overwhelming You're already overwhelmed. Short and to the point, yet compassionate is what I aimed for. And lack of trust in your doctor. That's a really big deal, because you need to be able to communicate with your doctor, and so I really do go into a lot of steps on how to address that, but address it in a way that's comfortable. As you can see, we're talking here about listening. Well, the power of being direct, respectful, polite, making your provider aware of changes in your body, writing down your questions, having a person with you, a second set of ears, understanding your diagnosis, understanding your treatment plan decision, getting a second opinion Everybody should do that. If nothing else, if it agrees with your current treatment plan, it gives you confidence in your current treatment plan. Asking for tumor board review of your diagnosis. Give your mind a break, practicing mindfulness, accept responsibility for your personal wellness decisions. That's also a keystone of self-advocacy. Most of you, I'm sure, track your tumor markers, your lab work, writing down talking points, if anticipating a tough conversation, and approach a tough conversation with the intent for a positive outcome. And it goes into that because if you have that mindset of, okay, I'm writing down these talking points and there's a journal for that, and then approach it with an intent for a positive outcome, even if you don't end up with a positive outcome in that particular conversation, more than likely you're going to end up with a positive outcome down the road because of how you handled yourself. Build a strong cancer care team, work with your HR department or leave administrator that's tough for everyone and understanding your health insurance benefits. We go into deciding on a treatment plan. If you're a childbearing age, wrapping your head around your treatment plan which, brad, we just talked about be prepared for a change in plans.
Jill Squire:Important, shareables, based on my navigation and case management experience dealing with an ostomy and dealing with a feeding too, because people have a lot of fear about those two things and it's a reassuring narrative about both of those and why. And sources to go to of other people that have had both of those, that live very full lives. It's not just a positivity website. It is truly people that have had either of those and really give in-depth insight into what it's like. They'll answer questions and so on. Insight into what it's like, that will answer questions and so on. Credible sources for information.
Jill Squire:Symptom management, the power of rehabilitation and prehabilitation, pelvic floor physical therapy, which is huge. Palliative care I'm going to be adding a chapter on integrative health and integrative oncology and then vaginal stenosis with radiation therapy or surgery. Your oncology team members can be super teammates. Deciding to no longer have treatment does not mean stop living life. That's a really tough conversation to have with your family, but they're not living in your shoes. It takes a lot of thought on your part to put forth what's important to you in that moment, what advanced directives, living wills and substitute decision makers are. And in closing we have our journal table of contents, and these are about 20 different guided journals. That sounds like a lot, but it really does take a lot of stress off of you because everything is very well organized and you can find it immediately. This is a draft, so you have to excuse me, because it's actually much prettier in the book.
G van Londen:But I also think, jill, that this is very helpful. Even if you, as the patient, are not strong enough to fill this out, somebody else can fill this out for you and you can use it when you're feeling better as a way to look back at what happened with me at those times. How was I doing, what treatments did I get so sort of a way to document and look back at later.
Jill Squire:Yes, and they're all designed to be easy, as you saw, dr Van London, to fill out. They're intentionally designed not to be overwhelming and I took care to make sure of that in the design of these. I had survivors review this prior to publishing it and it was also medically reviewed by a board-certified hematologist and oncologist also medically reviewed by board-certified hematologists and oncologists. All of the steps in self-advocacy are evidence-based. I have resources that back everything up. It's fairly comprehensive. In practicing empowerment and self-advocacy, one of the things I'd like to go to is what is important to you journal and then talking points for conversations with those you hold dear. So that's a really compassionate way to put that, because you're anticipating possibly a tough conversation, but if you say with those you hold dear, that's a compassionate way of putting that right. And so that is the approach is to help you feel like you have a friend with you through this journey. Go ahead, jen. What were you going to say?
Jen Kehm:no, I just think you're only with your physician for a short period of time, so having the opportunity to give them more data and information is really powerful yes, so I'll take you for to that point.
Jill Squire:I'll take you to the daily check-in and then also your questions for your physician, because it's really important to write them down and that is incredibly important to do. Okay, there we go. Questions for your healthcare team, date, physician, provider, name, your question, and that there's a space for your answer so you can write down the question for your answer. Now let's say that you chicken out. While you're in your meeting with your oncologist, you can look down at your question instead of maintaining eye contact and read it off. That can give you a sense of empowerment and it gives you a break from their boring eyes. Or you can tell them a pun and see if you can get them to laugh and then ask your question. Or, if you've brought someone with you, you can ask them to read the question for you. So there's a couple different things to do to have that question answered. Or you can ask if they have a scribe, like a nurse, with them, or you can ask someone to come into the room with you and ask the question for you if you're chickening out. But it's really important that you ask it because this is your diagnosis, your treatment, it's your life and if you think of it that way, I think you hopefully will feel more empowered.
Jill Squire:One of my watershed moments in the past six months that made me realize how difficult empowerment is for many people in this space, in spite of this book being put together, is a PhD in public health in my particular group and a physician both said in our group is not just to me, it was in a general discussion, but I heard it I'm terrified to ask my oncologist questions. They both know the questions to ask and I asked why. We don't want to make them mad. We don't want them to think we're stupid.
Jill Squire:The research I want to do is there's two grants I'm writing, but one of them is to work with cohorts of people on this material, have a valid survey before and after on their comfort with self-advocacy, their sense of empowerment, and check in with them one month, two months, four months, six months. Also, take their comments about what it feels like to be in that provider office, that healthcare team member office, and collate them with the publication of the other results in a way that we can make the providers, the healthcare team members, aware of how the patient feels, how the survivor feels, sitting in the office. Because I think if we set that awareness up in an evidence-based publication and we do some very simple workshops around that and publish it in an evidence-based journal, I think just having that awareness and then having some conversations around how can we change the narrative in that appointment could really make a big difference in empowerment for those survivors?
G van Londen:Yes, when this grant gets awarded. Is this a study that you were talking about? Yes, and you will be recruiting through. How will you?
Jill Squire:were talking about. Yes, and you will be recruiting through. How will you? So I actually talked with the gathering place and I was going to approach Cancer Bridges to see if we could work with cohorts of people there, and the gathering place is in Cleveland, they're two hours from me. Yes, and they send people into underserved communities. I had a brief conversation with them about me actually accompanying their social workers into underserved communities, to workerved communities. I had a brief conversation with them about me actually accompanying their social workers into underserved communities to work with them there, which to me would be tremendous.
G van Londen:But that means for the people here listening later on the podcast, there's the possibility that they could participate in your research as they wanted to.
Jill Squire:Yes, and then I know we're running out of time here. Daily check is just so you can take your pencil and mark how your day is going, when you're having a particularly good day or a particularly bad day. This will help you with your conversations with your physician and tracking what is happening with your symptoms. Pain is not just pain. The nature of the pain is really important. I actually just interviewed a rheumatologist who is an oncology rheumatologist. She said this is so important, especially with the immune checkpoint inhibitors, to understand the nature of the pain. Immune checkpoint inhibitors to understand the nature of the pain. It's important with neuropathy. This helps you distinguish it and describe it to your doctor. You can mark when it's happening, how it's happening. If you're having diarrhea, the nature of it is really important. You can say what days it's happening and how many times in 24 hours. How much were you able to eat? How much were you able to drink? Exercise is so important. What were your concerns that day? What did you enjoy doing today?
G van Londen:Even if you haven't had the energy to fill it out. That says something, too, when you're reviewing your diary, this workbook, to prepare for your doctor's appointment, not having filled it out. It says something about how you felt, either very bad or very good.
Jill Squire:Just write it in for the date so you can see that there's an entire week on a page spread nauseated, all day and just a smiley face or whatever you want to do. But you can write your appointments in here. There's a place to write down what's important to you. We were talking about shared decision making. To one woman, her faith was important. To the gentleman, going to work was important, and then the talking points surrounding that, so you can express yourself to your family and healthcare team. Very good.
G van Londen:Jill, I'm very impressed. I have a question If you wouldn't mind going to a topic we can discuss with the remainder of our time, which is step 10, trust, because I think, as a provider and as a patient and Brad has been a patient we've had tons of issues with trust on both sides of the table and I thought that might be a good topic for today, because this topic, compared to all the other other topics, is the largest content. It's practically a whole page. So let's go over this and fill the rest of the time. And we have a question Somebody's asking is the book available electronically? Go ahead, jill.
Jill Squire:At the end of the month it will be, and so it's available in paper right now. I will say, if you want to use the journals, the paper version will be much less expensive than printing off the journals yourself. I can guarantee you of that. The paper version is $27.97 and it's like 8 by 11. It's regular page sizes so it's easy to use. I'm going to be making a smaller paper version, but I'll be making an electronic version and then people that don't read things like this quite as well and read a narrative version better, and where there's a case example of beach, like we talked about, I'll be making a narrative version, probably in October, to publish for the steps in advocacy self-advocacy as well, for the steps in advocacy self-advocacy as well, wow, I'm hopeful that helps answer the question.
G van Londen:So step 10 is about addressing the lack of trust in your doctor. I don't know what's the best way of doing this. Jill, reading this from top to bottom is probably not the best way to spend our time. Is it possible that you summarize it perhaps in a few minutes? Absolutely.
Jill Squire:Usually it's a misunderstanding Not always, but usually and usually especially if you have moral support with you or if you're able to talk with somebody else in the office, it can be resolved. But not always. And if you're still uncomfortable, you need to find a different provider, whether it's another provider in the office or another practice that you feel is just as good in your specialty. That's really important too, but you have to feel free to communicate with your provider. That's imperative because advocating for yourself, communicating with yourself, is imperative.
Jill Squire:What you can do is if there is an advanced practitioner, such as a physician assistant or a CRMP, that you trust, you can see them instead and they can communicate with your provider. But you certainly can ask to switch to a different provider in the office or a different. If it's a CRP or a PA that you're having an issue with, you can ask to switch to a different one in that same office. I hope that helps and do not delay your treatment or skip a treatment because of this, because that can affect your outcome. So still go and have your treatments while you're switching providers and you can work with your insurer and you can reach out to your insurance company to find someone who, if it's not working in that practice, to find someone what you're alluding?
G van Londen:to is that your connection with your provider is a relationship.
G van Londen:Yes, provider is a relationship, and any relationship can have an issue at some point, and I think what is important that Jill describes is to pause and take a step back a second and look at what is going on here, For example, patients were angry with me because they were not able to reach me or I never answered them, but I did not know that they were not able to reach me, or I never answered them but I did not know that they were even trying to find me. And so I would try to explore why something happens, try to see if whatever happened can be improved upon sort of a negotiation and exploration and, depending on how they respond and maybe you give them a trial period then decide if you can stay with them and give them a second chance or if you have to switch. And all of this can be difficult because if you're in a city it's different than when you live in a rural area where you're really dependent on maybe one provider. If you're switching to a provider, another provider, same office you don't have to explain yourself. You just want to switch and that should be it. Sometimes individuals get a little bit of pushback from the staff, but you should not have to explain yourself and they should not give you any resistance switching to another provider in the same office. If you need records to go from one office to the other, that should just happen without you needing to explain why. Medical record office. Anyway, these medical records are not handled by the particular office anymore.
G van Londen:But I think this is very relevant because, depending on how you trust your provider, you feel better about sharing what's going on with you, you can address your concerns more thoroughly, you make better decisions, you feel at peace about the path you've chosen. At the end of the day, that makes your soul feel good. And if you don't have that click with your provider, it can really cost you numerous nights of loss of sleep and concern and stress that none of us need. We already have enough on our plate. I think that is my nutshell. I was gonna ask greg because I know he he's had his fair share of trust for good and bad with providers. I don't know how comfortable you feel sharing anything, but you don't have to.
Brad Buchanan:I'm putting you in the spot here well, yeah, I mean I've dealt with the dozens and dozens of different doctors and, yeah, some of them I don't feel understood the nature of my diseases. So I mean I strongly echo what's already been said about getting a second opinion. I also I was in the hospital for like extended periods and I was getting to the point where I was like they would come to me and ask which nurses do you want? Because I was in very intensive daily contact with nurses and I didn't know you could say I don't want Nurse X. On the case today, if there'd been problems or there was a lack of trust or whatever it was, I'm hoping that most patients never get that I had the power to say no, nurse X doesn't do a good job of accessing my port line or whatever. So yeah, I think patients have a lot more autonomy in some ways than they know.
Brad Buchanan:But I will say it's important to recognize that there are differences in levels of expertise and seniority and what I would always say is, if you're getting bad news from someone who is junior to the usual people that you talk, to wait until you hear from their boss or the person who's in charge, because there was one experience in particular where a junior doctor came in and decided to unload some what he thought was bad news that I needed to hear. He ended up being wrong. I made a bit of a fuss and said you know, next time you have bad news to tell me, bring in my actual doctor who's in charge and who is senior to this junior fellow, so that I'm hearing it from the person with the most authority, the most experience. But yeah, this is a tough issue. It's also an emotional issue because when we feel our trust has been betrayed or misplaced in our medical team, it's very upsetting and it takes a lot to get over that. But that maybe is another issue.
G van Londen:Yes, by no means can we satisfy this topic in the little time we have, but I thought this might be a good topic maybe to end with for today at least.
Jill Squire:I was just going to say that I thought a good way to end this. But I'm happy to take questions or listen to questions. Oh, here's a fun post. Yes, here's the fun. I thought we could end on a pun. And what did the pencil sharpener say to the pencil? Stop going in circles and get to the point. So if you're having a really intense conversation and people are starting to get at each other's throats, or with a family discussion, or you have a doctor who never smiles, you can pull this out, or you just need to uplift yourself, or you have kids visiting you and you need a way to entertain them, you can pull the last two pages of this out.
G van Londen:I like this. It brought a smile to my face. Thank you, jill. I thank you everybody. This is a different kind of book than we usually do, but I thought this book is great for you or anybody else who hopefully never has to go down this journey. Thank you, jill, for doing this. I have a feeling we will hear more of you in the near future. Just keep us posted if we can help you with the recruitment.
Jill Squire:Thank you for having me. It means a lot, it really does and thank you for all your praise.



