CancerSurvivorMD®
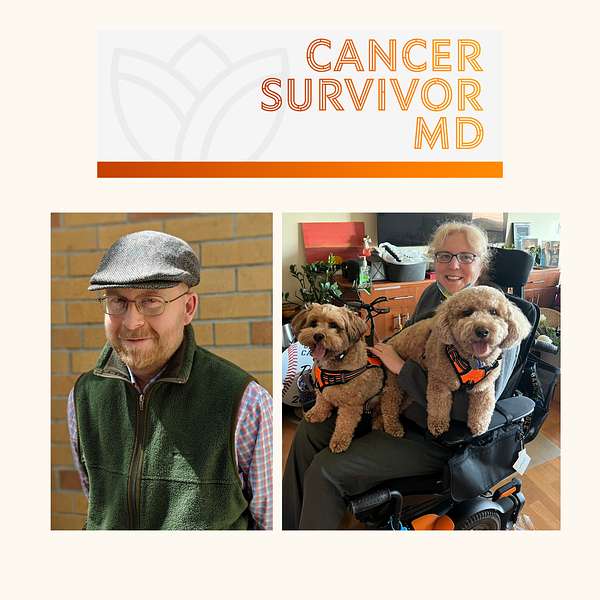
Hello! Welcome to CancerSurvivorMD’s podcast by Brad and Josie!
We will share our experiences with living in sickness, health, and anything in between to allow healing and growth. The topics will focus on cancer survivors and caregivers but will likely resonate with anyone who has been diagnosed with any health condition.
Brad is a retired English professor and cancer survivor, now a facilitator of the Writing as Healing workshop.
Josie is a retired medical oncologist and cancer survivor.
If you have any questions or topic suggestions, please send them our way, and we will try to incorporate your request.
Please take a look at the disclaimers (https://cancersurvivormd.org/disclaimers). Words can hurt—if you feel you might get or have been triggered, please stop listening and seek support.
CancerSurvivorMD®
Brad and Josie - Cancer Recurrence
How do you navigate the turbulent waters of cancer recurrence and its treatment?
In this emotionally charged episode, we share deeply personal stories of battling persistent abnormal cells, undergoing numerous medical procedures (surgery, radiation, and stem cell transplant), and the heart-wrenching decision to opt for treatments that come at large risk of loss of fertility, loss of life, and loss of quality of life. We will discuss the unique nature of each of our cancer journeys (Brad's lymphoma and Josie's solid tumor), all through the lens of lived experiences. Prevention strategies are also discussed.
Helpful links:
https://www.cdc.gov/hpv/parents/vaccine-for-hpv.html
https://bethematch.org/transplant-basics/how-blood-stem-cell-transplants-work/how-donors-and-patients-are-matched/
https://www.cancer.org/cancer/managing-cancer/treatment-types/stem-cell-transplant/types-of-transplants.html
- Disclaimers: https://cancersurvivormd.org/disclaimers/
- Brad Buchanan: https://linktr.ee/bradthechimera
- G [Josie] van Londen: https://linktr.ee/cancersurvivormd
- CancerBridges: https://cancerbridges.org/
Good morning Brad.
Brad Buchanan:Good afternoon, Joey.
G [Josie] van Londen:Well, we've talked a lot about our initial cancer treatment, so I think we're both ready to talk about our experiences with cancer recurrence.
Brad Buchanan:Yeah, I think so.
G [Josie] van Londen:My story is a little longer this time. Would you like to go first? No, no, no, no no so then I'm going first, okay my story is probably even longer, but we'll see.
G [Josie] van Londen:We'll compare length of stories so my story picks up where we left off in terms of that. They removed the superficial layer of my cervix and the hope was that I would build immunity to HPV. That would have been it, but it wasn't. I can't remember. As I've said before, this is 20 years ago. They put me on a frequency of repeat pup smears. Frequency of repeat pup smears and the timing of these pup smears varied depending on what they found, and they found continuously, almost practically what I can remember abnormal cells that were low or high grade dysplastic over the course of years, which was nerve-wracking because it means that I had to do the math to calculate when I would see the doctor, how long it would take for the test results to come back, how long it would take for them to need to do a procedure, and I had to then calculate whether or not I will be on some heavy duty clinical rotation. So it was a little complicated to balance all of that because I never disclosed anything to anybody, not even my own family. We've talked about it before. I thought I could handle this all easily on my own. So they kept burning, they kept ablating until it went into the cervical canal, toward the inside of the uterus and they felt they couldn't monitor it well enough anymore, that we needed to do something more, which, at that point in 2011, was a hysterectomy. And then I thought and I hoped okay, well, now it's history, because the cervix is gone, but they keep watching the rest of your gyne tracts, which, for somebody who is at an abnormal POPs in the past, is something that continues to go on for the rest of your gyne tracts. Which, for somebody who has had an abnormal pop smear in the past, is something that continues to go on for the rest of your life. So they kept watching and a few years later, maybe two years later, abnormal cells popped up based on at this point, it's a vaginal smear. Cells popped up based on at this point, it's a vaginal smear, and that triggered a whole repeat cycle of ongoing smear positivity, ongoing surgery to chop the vagina shorter and shorter until there was nothing left to chop. I realize this is maybe somewhat graphical and maybe that's my way of dealing with this, but that last procedure where they cut as much as they could using a magnifying device guided by a solution that highlights abnormal cells without causing me a lot of bowel and bladder complications.
G [Josie] van Londen:The pathology showed that there were positive margins and that there was invasive cancer detected. So that was interesting because they couldn't really operate anymore. So then they discussed my case in tumor ward and the consensus was let's try radiation. So they tried brachytherapy, which is a localized form of radiation that doesn't have a lot of depth coverage, and that meant that they had to insert a radiation probe into the shortened vagina. That had to sit there for what felt like 30 minutes of frequency of three times a week for a few weeks for it to have an effect. Obviously, the typical radiation side effects of skin burn, pain, irritation, highly uncomfortable.
G [Josie] van Londen:The dilemma was if, on top of that, we needed to add external radiation. The external radiation was an agonizing decision process Because I was right on the cusp of two guideline algorithms. You could make a case for it to be added. You could make a case for it that I didn't exactly qualify and at that point I was working as an oncologist, I had finished my medical training, I had joined the faculty as a medical oncologist, and so that decision came very close to my own personal situation. Now, trying to figure out how am I going to decide as a doctor, as a patient, do I trust the doctor in deciding for me.
G [Josie] van Londen:I remember at one point my doctor had said if it ever should get to that point, we can always add a little bit of radiation. And those words we talked about it in the last episode that words can have a huge power. Those words stuck with me a lot, because to me a little radiation is first of all. There is no little radiation. What is little, I guess? And radiation is not a minor cancer treatment, it is an entity on its own, it's a discipline on its own that deserves a place in the arsenal of treatments we have to combat short-term, long-term. And so I never really appreciated those words. But here we are. I needed radiation and a big decision back and forth.
G [Josie] van Londen:Eventually I decided with the radiation oncologist it was not to do the external radiation. And the major reason that I remember which is, I guess, maybe what matters most in my head for me in my situation is that if the cancer should reoccur again, that they probably cannot do more radiation at that point and I wanted to have one more local original treatment in my arsenal in the future. They really couldn't operate without causing a lot of morbidity, so I wanted to reserve one more local treatment in case it was needed. So that was my reasoning for let's not do external radiation that covers my whole pelvic. Let's leave that to have it in my backpack. But please remember that every cancer and every subtype of cancer is unique and decision-making is highly personalized. For some cancers and subtypes of cancers it's really important to maximize upfront treatment to reduce a recurrence risk, because at that point it becomes incurable. In my particular case, the tumor had proven itself to be locally persistent. Tumor had proven itself to be locally persistent, and so I wanted to hold on to more future local therapy options, if that makes sense, anticipating that it will recur again. So that is where that stands.
G [Josie] van Londen:I finished my brachytherapy, which I think what I did because all of this is very, very deeply. I had to go in, I think, three times a week for a few weeks to have a whole procedure done. Each time I went in that lasted about maybe three hours. They had to insert the probe in a way that was precise, and so they had to insert this every time in a CT scan, and then I wasn't allowed to move because otherwise the probe would have moved and the radiation wouldn't be exactly administered the way it needed to. So it was very interesting how they moved me from one table to the other table. They sort of did that for me with a very interesting contraption. So I didn't move my pelvis and that probe wouldn't move. It was a whole ceremony like unbelievable, and I had never realized that before. So that was eye-opening to me.
Brad Buchanan:I'm sure it was extremely uncomfortable.
G [Josie] van Londen:Oh yeah, the whole thing was absolutely. And then you lay there on your own. I don't even know how long I was laying in the room there. It felt like an eternity. Every time it was dark I was laying in the room there. It felt like an eternity. Every time it was dark, I was alone and you just have to lay there and sort of. I guess I dissociated. I kind of took myself out of the room because it was really not pleasant.
G [Josie] van Londen:But once I was healed from that, I decided I'm really, really really going to now figure out why I keep having this. And that's where the story comes in that I discovered that I have an immunodeficiency by getting support from people who donate their blood, and therefore their antibodies, to me so I can infuse them on a weekly basis to help my immune system fight HPV. I haven't had an abnormal lesion in my gyne track since, and so that ended that in 2017. So the whole thing had been going on for almost 17 years and I wish, I wish I would have known all this way much earlier. Then I didn't have to deal with all this and complications which which we, depending on how today's session goes, we might discuss in a future episode, but that is my story. There's more to the story, but I'll stop here, I think, for now.
Brad Buchanan:Do you mind if I ask a couple of questions? No, so do you now consider that it was probably a good idea to not have that bigger external radiation of the whole pelvic area, that in the end it was not going to be necessary?
G [Josie] van Londen:Yeah. Yeah, in hindsight, but it was a very, very difficult decision to make.
Brad Buchanan:Yeah, it sounds like it. Then Medical training helped you to make a better decision.
G [Josie] van Londen:Yeah.
Brad Buchanan:Or was it sort of a gut level thing?
G [Josie] van Londen:In the end I think I have to say it was my guts.
Brad Buchanan:Yeah.
G [Josie] van Londen:You can reason yourself through it, but you can reason in two directions, because I fell exactly right on the cusp. I guess I did reason with myself is that I said to myself I want to hold on to it, so I have this treatment for later. Right, but I don't know. Can you ever separate a decision from your guts? I think. I think you never really only make a decision only with your brain or only with your gut or your emotion. I think it. I think it's never isolated, it's a combination of the two.
G [Josie] van Londen:I think, Plus, education and knowledge is power, but sometimes ignorance is bliss. So I guess it's all about balance. And, lastly, you can't treat yourself because you're too close to it and the stakes are too high. This is about your own life, and so it can lead to desperation if you try to make a decision for yourself. It's rather difficult for anybody, but in particular, I think if you are a health care provider, and in particular, a health care provider with expertise in the field that relates to the illness you have if this makes sense yeah, no, that makes sense, but yeah, it sounds like.
Brad Buchanan:Well, I'm glad that it was the right decision ultimately to to hold back on that, and maybe that's an example where you know, choosing to err on the side of undertreating right and hoping that that will be sufficient, rather than overtreat immediately and deal with all the fallout that that comes that.
G [Josie] van Londen:But it all depends on the situation. Sorry, I cut you off. Some tumors you need to jump on because they're somewhat more aggressive and prone to systemic spread. In my particular case, had shown itself to be indolent, but persistent and recurrent, and so my hope was if natural course continues this pattern and it will stay in its place, then I have one more local treatment option to buy myself extra time. One more local treatment option to buy myself extra time. But every person has to make their own decisions, informed by their providers. Even indolent, slow-growing tumors that continue to grow slowly despite multiple lines of cancer therapies can result in death, even benign tumors that are compressing the surrounding tissue, and so every situation is highly unique. In conclusion, I think it's a highly individualized treatment decision-making.
Brad Buchanan:In my case, yeah, and your doctors were going to respect your decision either way.
G [Josie] van Londen:Yeah, I was cognitively intact, meaning I'm making the decision, fully aware of the pros and cons of my decision, and this particular person was my colleague and I sent my patient to this particular person. So that makes the discussion a little complicated, because now, am I his equal, am I his patient? So that made it hard for me to talk and there wasn't really anybody else who was doing it, so I couldn't really go to anybody else within our system, and within our system that's the only place where I had insurance coverage. So I were really was limited in where I could go for a second opinion.
Brad Buchanan:Yeah.
G [Josie] van Londen:But nevertheless I trusted him taking care of my patients. I valued his way of thinking and he was leaning against external radiation, but he would do whatever I feel comfortable with, which you know. Put it for a while on my lap. What am I going to do now?
Brad Buchanan:Yeah.
G [Josie] van Londen:Yeah Well, again a tough decision, but for children of any gender, starting at age 11 or 12 years, you can vaccinate them with an HPV immunization that will greatly reduce their risk of developing an HPV-related cancer. There's two dosages, six to 12 months apart. There's two dosages six to 12 months apart. I'm looking here at the CDC website. It can even start at age nine. Early protection works the best. Teens and young adults can be vaccinated too.
G [Josie] van Londen:The CDC here is saying that HPV immunization is not recommended for everyone older than age 26,.
G [Josie] van Londen:It is not recommended for everyone older than age 26, but it can be given for those age 27 through 45, after having discussed the pros and cons with their doctor.
G [Josie] van Londen:There's apparently less benefit for adults compared to younger individuals, and the reasoning is that these individuals often have been exposed to HPV already. There's some benefit as a secondary prevention after somebody has already developed an HPV related cancer. In very unique situations there's some benefit, and so also for this I would certainly discuss the pros and cons with your cancer doctor, and it may not be covered by your insurance in this particular situation prevent 100% the development of any HPV-related issues, but it will definitely reduce it both from it happening as well as the severity of any problems you might develop. Nothing in medicine, I guess, is 100%, and so, despite having had HPV immunizations, one still needs to stick with the appropriate monitoring guidelines, and because HPV is so highly prevalent in our society, almost everybody has been touched by it. It will be very helpful for everybody to get these immunizations, both to help yourself as well as help society as a whole.
Brad Buchanan:Yeah, okay, well, yeah, I remember both my daughters were vaccinated for it when they became old enough, and I was amazed and delighted that you know we're able to vaccinate for some form of cancer, right? I mean, that's what's going on here. I don't know if you know any more about, like new vaccines that might preempt other types of cancer, or you know what is the state of research in that domain, like vaccinations against this kind of thing in general.
G [Josie] van Londen:I think this is a clear example of a very clinical application of primary prevention of a cancer, meaning preventing it from happening to begin with. Yeah, but there are immunizations that are in research application. I don't believe that they're really ready yet to be applied in the clinical arena, where immunizations are being used in those who have been diagnosed with cancer to help their treatment, to boost their own immune system, to fight the cancer they've been diagnosed with. So, that would be sort of secondary, tertiary line of prevention, if you call that that way.
Brad Buchanan:Yeah, what does HPV stand for, anyway, if you don't know? Oh yeah, hpv human papillomavirus. Okay, well, thank you, that's good to know. Do they know how is it transmitted?
G [Josie] van Londen:Yes, HPV is spread through intimate skin-to-skin contact. You can get HPV by having vaginal, anal or oral sex with someone who has the virus. Even if they don't have signs or symptoms, Nearly everyone will get HPV at some point in their lives. Most HPV infections will go away by themselves within two years, but sometimes in some people HPV infections will last longer and cause some cancers.
Brad Buchanan:Okay, but for people with a robust immune system, does this type of virus pose a serious health risk, or is it mainly for people with an immune deficiency? Does it lead to cancer? For instance, I had and I'm jumping the gun a little bit, but after my transplant I had a post-transplant lymphoproliferative disorder, also brought on by a virus, the Epstein-Barr virus. That I think probably was in my brother's immune system and it wasn't doing him any harm, but when I got it it was doing me. Yeah, it basically produced a lateral lymphoma in my body and I'll go into more detail about that. But yeah, so viruses that cause cancer. If we can vaccinate against the virus, then we kind of do an end run around cancer and just avoid it entirely, right? That's kind of the principle I'm seeing here.
G [Josie] van Londen:Yes, so HPV human papillomavirus, which is different from EBV, which you will be talking about.
G [Josie] van Londen:Hpv infections, as I mentioned, happen in almost everyone, but only in a small proportion of people does it result in the development of cancer, which can take years and sometimes even decades to develop.
G [Josie] van Londen:Hpv vaccination can prevent over 90% of cancers caused by HPV. There are some risk factors for being less able to fight off or clear HPV infections and be more likely to develop health problems caused by HPV. Those are, for example, smoking, as well as having a weakened immune system, such as people living with HIV or AIDS, or maybe even, by extrapolation, those who have prolonged states of immunodeficiency because of cancer treatments. But there's no way to know who will develop cancer or other health problems from HPV at this current time, and so more research needs to be done. But there's a huge stigma on this, because it's deemed to be your own fault or you must have had multiple partners and so you've done this to yourself, type of thing, which is obviously not the case. That's a very stigmatized view that I hope will disappear. And lastly, I would like to add, for those that have a chronically HPV positive state, they may want to discuss the pros and cons of anal cancer screening, since recommendations are slowly starting to change.
Brad Buchanan:to add that Honestly, I think this is important information, since it's such a common virus and, you know, can have pretty bad consequences for some people anyway. And you know I don't know, maybe the people listening to this right now, since they may have had cancer or had some other health problem that it's important for them to know this kind of thing. I am at a point in my life where there's no such thing as too much information, you know, with respect to health. Even if, yeah, even if it's, you know, something that I don't currently have wrong with me, I think it's just important to have all the information you could possibly have. And, yeah, as someone who's had a compromised immune system for a long time, I realized that there are a lot of viruses out there I needed to be very aware of and to avoid if I possibly could. Thank you, dr Judy.
G [Josie] van Londen:Slow. Maybe that's enough for me for today.
Brad Buchanan:All right, okay, so my story of recurrence of cancer basically, after I got my initial somewhat violent chemo treatment for my lymphoma that had burrowed into my lung and created a tumor that burst and sent me to the hospital, I got five more cycles of chemotherapy over the summer of 2015. And at that point they were talking about preparing me for an autologous stem cell transplant, which would have been maybe in October of 2015, because they were fairly certain that the chemotherapy wasn't going to put me into lasting remission on its own. So, yeah, I got my last cycle of chemotherapy, I think in late August or early September of 2015. And then we started thinking about preparing me for the, the stem cell transplant where I would donate my own stem cells and I was, uh, just about to go in to pick up the. I think it's the neupogen shots that you need to give yourself so you start producing lots and lots of stem cells to give yourself, so that you start producing lots and lots of stem cells that they put into storage so that you can then re-donate them to yourself after you've had the.
Brad Buchanan:Whatever the prep regimen was going to be in that case, I think the prep regimen probably would have been chemo and some radiation, although we never got that far, because, you know, I started noticing that the same little lumps had come back on my body, the lumps that had signified my original lymphoma that you know. It took them six months to figure out what they were and finally diagnosed me. They were back with a vengeance, and so I just said let's stop everything. And because I think the lumps are back and and of course, I got another pet scan where it showed that, indeed, kind of the pet can lit up like a christmas tree, as they put it. This is late september, early october, I think of 2015 yeah, the lumps were back very quickly and again, you know, it might have been one of those cases where they what the chemo had accomplished was to neutralize the weaker cancer cells and galvanize the more aggressive cancer cells, because all of a sudden, my you know my cancer, which had started out as slow moving, right indolent, all of a sudden it had come back very quickly indeed and was now suddenly extremely aggressive. So that was a real wake-up call to everybody. My medical team was, of course, dismayed and surprised. We got to a stage where we happened in early November there's often an October surprise that comes out. Some event happened that is intended to affect public opinion, you know, for or against the sitting president and the party in power. So that's where that phrase October surprise comes from.
Brad Buchanan:So anyway, yeah, so we had to pivot very quickly from the plan of the autologous stem cell transplant to the allogeneic stem cell transplant and find me a donor. Unfortunately, I'd already talked to my brother James, who was a doctor in the hospital, and he said you know, I'm going to have to do this, I'm going to have to do this, I'm going to have to do this, I'm going to have to do this, I'm going to have to do this. I'm cell transplant to the allogeneic stem cell transplant and find me a donor. Unfortunately, I'd already talked to my brother James, who is, you know, just a year and a bit younger than me, and I said you know, hey, you might well end up being the best chance I have if I can't do this version of the stem cell transplant where I donate my own cells. You know that we're going to ask you to take the genetic test and so forth to to see if you could be my donor.
Brad Buchanan:But you know, the unspoken subtext of all this was we went from a plan to have the stem cell transplant be a fairly safe, relatively low risk procedure where you're your own donor, right.
Brad Buchanan:So the possibility of having acute graft-versus-host disease from your own stem cells is pretty small, I know, if not negligible.
Brad Buchanan:So we realize that, yeah, now I need to have the much more dangerous, difficult version of the stem cell transplant where you're going to have to give me total body irradiation as well as comprehensive, a last big dose or two of chemotherapy to try to reduce the cancer completely and essentially get rid of my old immune system, which had showed by that point that it was incompetent to deal with my renal blood cancer anymore. It was just completely useless where that was concerned. So that's when we went into prep mode for an early 2016 stem cell transplant and my brother turned out to be a 10 out of 10 genetic match. A younger male sibling donor is considered the best option anyway for biological reasons not just sheer sexism, but anyway and he was more than willing and able to help. But, yeah, my cancer came back with a frightening rapidity and vehemence that meant that we had to quickly shift gears and go into prep for a much more difficult, potentially deadly transplant. So any questions?
G [Josie] van Londen:Many Tell me again when was the day of infusion? Do you remember the date? When were you actually infused with your brother's cells?
Brad Buchanan:I think it was january 11th, so about four months later yeah, okay.
Brad Buchanan:So yeah, I was on january 3rd and it was eight days of prep, of chemo and total body irradiation I think, for six of those days, then a couple of rest days maybe on either side of that, and then he came to donate his cells and we played chess in my isolation room and then, yeah, I got his cells on. We played chess in my isolation room and then, yeah, I got his cells on january 11th. So just it was so stressful getting to that point where he, you know, once he had been determined been determined that he was going to be my donor, making sure that he got back in time to donate millions of stem cells. You know, we talked a little bit about this on the interview we did, where I was paranoid that something would happen to him on his way back A very selfish paranoia really that his plane would crash and then I'd be left without a donor and meanwhile he would be dead. So and he, he told me, just before the transplant happened, he, he said that my nurse coordinator, who had been engineering all the logistics of the transplant, she gave him a little pep talk after his visit, he came and visited sacramento to to take the final genetic tests and just be kind of thoroughly vetted from a medical point of view, yeah, and she took him aside during that visit and said you know, at some point we're going to take brad past the point of no return with all this chemo and all this radiation.
Brad Buchanan:So if he does not get your stem cells after that, then he will simply die. So if you're going to back out of this at any point, back out now, because at a certain point it will be too late, and you know he he didn't back out, thankfully, but yeah, he shared that story with me, I think, as I was driving him to the airport to send him back to Montreal where he was living. And that was quite a parting message to the liver that the next time you see me, brad, you know I'll be the only person on the planet who can save you. So that was quite something. Time you see me, brad, you know I'll be the only person on the planet who can save you. So that was quite something. And, needless to say, you know the emotions that I feel towards him now are extremely powerful and I'm so full of gratitude it's hard to express. But again, from the transplant there were complications that we will have to get into.
G [Josie] van Londen:Yes, I wanted to ask but you already alluded to it a little bit how it has changed your relationship with your brother. But you said it's hard to describe, which I can understand, and maybe we can do it in a future episode to give me some time to think about it.
Brad Buchanan:But if somebody does something so big for you, yeah, and without so much as a second thought or a pause or any decision-making period whatsoever. It was just always yes, always yes. And you know being supportive throughout it. And you know he came to visit me again in the hospital when I was still extremely ill after the transplant, when I was blind. And you know I, I did, I did tell him.
Brad Buchanan:You know, before the transplant I remember walking to the hospital with him to say you know, there is a chance that I will, that I will die anyway from all of this, and I just want you to know that, like it's not your fault, like I enter into this procedure fully aware that I could prove fatal, and I've made plans to make sure that all my loose ends, my will, my advanced, you know, my last words to my children and so forth, have all been settled and written and and and put in a safe place so that I'm fully prepared in case this kills me and that you may experience some guilt if I do die. But that is not, it is not going to be your fault.
G [Josie] van Londen:Yeah, I was going to ask that, gonna ask that next how did he feel, did he? Did you later talk about this again when you about his guilt feeling, when you developed all these complications?
Brad Buchanan:we didn't really talk about that in my family. We didn't talk much about our feelings, I would say in general, you know, it was me, my brother, my dad and my mom, and my mom sort of did all the talking about all the feelings and we just kind of we were men and boys and so forth, so we just it kind of let sleeping dogs lie where that was concerned. I mean, I I have tried to express my feelings to him anytime, but he, he hasn't really opened up all that much about how he has felt about this whole thing. You know, I can only imagine but yeah, no, I'm, I have more than enough feelings about all this for both of us in some way yeah and yeah, I mean I've written a lot of poetry expressing that gratitude to him.
Brad Buchanan:You know, even ahead of time, just having this chance to live, you know, even if it didn't work out, just going into the transplant with a hopeful attitude, was so important that if it thing, you know, and things didn't go sideways pretty dramatically but they could have been way worse, even still but just going into the transplant with the idea that this really was, we were going to hit a home run or we were going to strike out, you know, like there should use that baseball analogy it was kind of all or nothing and I was just grateful to him for giving me that hope.
Brad Buchanan:You know that I wasn't going to die without a donor Like nobody does anymore, by the way, that they do transplants on people who are very much less well-matched on paper. And then then my brother and I were matched. I still don't know why I got such an acute case of graft-versus-nose disease. On paper it really shouldn't have happened. And they now test, I think, for 12 genetic markers and there's just 10. But yeah, they're pretty confident that they can rescue almost any patient, even if there's nasty graft-versus-nose disease. And I will say again what I will say later and what I've said before, that I was very unlucky to get such an acute case of graft-versus-nose disease.
G [Josie] van Londen:Most patients shouldn't expect that and I certainly didn't going into the to the transplant experience one of the things I guess I wanted to mean is the National Registry for stem cell donation it's the bone marrow registry, I believe thank you for bringing that up.
G [Josie] van Londen:I will put the link to the National Marrow Donor Program in the comments. I'm stuttering because the name has changed. It used to be called the National Marrow Donor Program, now it's called be the match and the website is be the matchorg, and their mission is to save lives through cell therapy, and this website is very comprehensive. It allows you to read about how donation works, why it's important to donate, how donors and patients are matched. There's information there about how you can advocate, how you can volunteer, how you can give, and so I think that's a very important point to bring up, because there is a huge need at national level for people to register both for solid organ, which you can do through your driver's license, as well as to be a donor for stem cell transplant. That is maybe a good opportunity here to raise some awareness for that, because there's a relative shortage of people who can donate, who have a very good match and are available within a short period of time, of all races and ethnicities.
Brad Buchanan:Yeah, the vast majority of donors in the database are white, european by ethnicity and so forth. So anyone who is not that. The need is especially urgent for some of your stem cells, for people who would really benefit from them. So, yeah, good idea.
G [Josie] van Londen:Correct. So it's a big story, brad, you fluffed it over very quickly and you thought you didn't have much to share, but you already almost talked half an hour.
Brad Buchanan:Well, yeah, you know the initial recurrence of my cancer, that you know the t-cell lymphoma, that that was originally diagnosed in a way that wasn't really much of a surprise. They they were never that confident. I don't think that they could put it into lasting remission without a transplant of some kind. You know, as soon as we, as soon as we realized it needed to be treated, they've always felt like it was going to be. It did respond initially to the treatment very well, very visibly right that the the first bolus of chemo had a huge effect on the cancer. But the cancer was sneaky, resilient and turned more aggressive as a result of, yeah, the treatments kind of transformed it and you could say, anyway, but I wasn't shocked that my cancer came back. I really wasn't shocked because of the way that they had prepared me to think about it and I and I always thought that the idea of me being my own stem cell donor sounded a little too good to be true. You know, I had sort of mentally prepared myself that I would need a donor.
G [Josie] van Londen:I think you're illustrating that blood cancers, lymphoma, lymph node cancers or their treatment philosophy is a little different from solid tumors. It's solid tumors. The primary intent is to get local control and potentially add systemic therapy for early stage disease to try to prevent a recurrence. But for lymph node and blood cancers like leukemia it's a fuse and so systemic therapy is a much more important upfront treatment modality. Sometimes they do add local control, but the treatment philosophy is rather different.
G [Josie] van Londen:One of the things I wanted to clarify that you said is I think the treatment escalated, selected out those clones that are more aggressive. That could be. It could also be, or it could both, be true that your tumor itself was transforming. Lymphomas are known to transform also spontaneously, and I don't know if the timing of that somehow was unfortunate and it looks like, but it is hard to know. Yeah, really, but it could be one or both.
G [Josie] van Londen:Chemotherapy works best for tumors that have fast dividing cells, although at the same time these tumors can have a high recurrence risk. But at least it will buy time. Every person decides differently if it's worth to go through the treatment. All we providers can do is follow the evidence, educate our patients to allow them to make an informed decision, weighing the pros and cons in the context of their life philosophy. Even if they make a decision that we would not have made, we have to respect that decision, as long as they're cognitively intact. One other thing I would like to add, which is the pet peeve of mine, is that every cancer is a cancer, no matter how large or how small or how slow or how fast growing. It's all scary.
Brad Buchanan:Well, and just my observations of my own disease in the beginning was it was confined to the surface of my skin for quite a long time and you know I didn't start coughing or feeling anything in my lung for months after I noticed those first blobs. So yeah, at some point clearly it did kind of transform from a skin, you know transform from a skin, you know, based or you know, subcutaneous they called it lymphoma to something that was much more, you know, aggressively targeting my organs and so forth. But just to get back to the types of transplant for a second, the type of transplant that he got was one where they did not give him the same total body radiation or systemic chemotherapy that I got. They didn't take him to the point of no return. In other words, they infused him with a new immune system that took over gradually from the old one, right. So instead of like being without an immune system, as I was, kind of like a boy, a bubble they let. The cancer never really went away and that gradual takeover from the new immune system for a while it definitely gave him a certain amount of remission, but somehow the cancer just kept mutating or outsmarting the new immune system somehow.
Brad Buchanan:And I have a feeling that if I'd had that type of transplant that that might have happened to me as well.
Brad Buchanan:Because, honestly, there's nothing I would have found more dismaying and horrendous than to have to keep worrying about a recurrence of my first cancer Because it was so weird and so enigmatic and unpredictable and kind of unclassifiable you know, they just ended up calling it Brad's lymphoma because it it didn't act like any other cancer that they'd really ever seen, apparently, and worrying about that recurring after a transplant would simply be a kind of an intolerable situation.
Brad Buchanan:So I I do feel like my decision to have this sort of conventional stem cell transplant where you do just blast away all the old immune system and all the you know, all the cancer in one fell swoop and then make room for a new immune system and risk you know acute graft-versus-host disease, because he didn't have much graft-versus-host disease when his immune system took over. There was much less of you know graft-versus-host effect than there was with me, you know graph for the most effect than I would for me. But anyway, I do think I made the right choice, even though it was extremely rough, because I don't worry about a recurrence of my first cancer. That's not on my mind.
G [Josie] van Londen:Yeah, that was a question I had. Do you still undergo surveillance testing? Do they still do scans? You're eight years out. Are they still doing bone marrow biopsies or anything on you at this point?
Brad Buchanan:No, thank goodness they're not. I mean, I do go in for blood tests every now and then where they monitor my lymphocytes and what have you. But yeah, those have been pretty much free and clear for years. Now I'm going to touch wood, you know, to nothing correct, nothing bad come, you know. But but yeah, I've since had many more things to worry about besides the the recurrence of my first cancer. You know, I've had blood cancer, number two, which was also deemed to be terminal until it wasn't, and then, of course, acute graphers, those disease that was much more painful and debilitating and than cancer had ever been at least. You know, from a sort of like, how I feel my body every day point of view. You know, I, having blood cancer, didn't feel like anything. You didn't feel sick, you didn't feel pain. You didn't feel pain, you didn't feel any type of, you know, you just couldn't notice. There were these funny little differences in your body, but they didn't seem to matter very much, you know.
G [Josie] van Londen:Well, no.
Brad Buchanan:And yet they did.
G [Josie] van Londen:Yeah, exactly, yeah, I don't know. But, I think this might be a good point, brad, to end here, and you did a very nice announcement of what we're going to talk about the next time, which is complications of our treatments, which, in your case, include Graf Rousseau's disease, the development of another lymphoma. So thank you all for listening. Stay tuned for that, and thank you, brent, for asking all those good questions and telling us your story.
Brad Buchanan:Yeah, well, thank you for answering my questions and telling your story as well.
G [Josie] van Londen:Thank you, brent. See you all the next time, all right.

