CancerSurvivorMD®
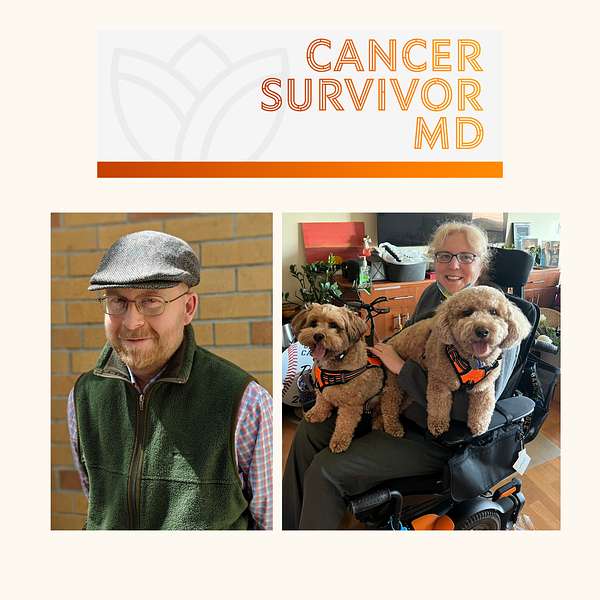
Hello! Welcome to CancerSurvivorMD’s podcast by Brad and Josie!
We will share our experiences with living in sickness, health, and anything in between to allow healing and growth. The topics will focus on cancer survivors and caregivers but will likely resonate with anyone who has been diagnosed with any health condition.
Brad is a retired English professor and cancer survivor, now a facilitator of the Writing as Healing workshop.
Josie is a retired medical oncologist and cancer survivor.
If you have any questions or topic suggestions, please send them our way, and we will try to incorporate your request.
Please take a look at the disclaimers (https://cancersurvivormd.org/disclaimers). Words can hurt—if you feel you might get or have been triggered, please stop listening and seek support.
CancerSurvivorMD®
Essential Elements of Cancer Survivorship Care: Screening for Secondary Cancers
Brad Buchanan, Colleen Dwyer, and I will discuss an essential aspect of cancer survivorship care. In this episode, we’ll focus on the importance of screening for secondary cancers among cancer survivors.
Relevant links pertinent to this episode:
- https://www.cancer.org/cancer/screening/american-cancer-society-guidelines-for-the-early-detection-of-cancer.html
- https://www.cdc.gov/cancer/prevention/screening.html
- https://www.cancer.gov/about-cancer/screening
General Links:
- Disclaimers: https://cancersurvivormd.org/disclaimers/
- Brad Buchanan: https://linktr.ee/bradthechimera
- G [Josie] van Londen: https://linktr.ee/cancersurvivormd
- CancerBridges: https://cancerbridges.org/
Screening for Secondary Cancers
===
[00:00:00] Introduction
---
[00:00:00]
[00:00:05] G van Londen (2): Hello everybody. Welcome to another episode of our podcast, and this time we have Colleen and Brad. And you've met them in the first episode, in which we talked about one of the five essential elements of cancer survivorship care. We talked about monitoring for cancer recurrence. This is the second episode in this series,
today we are going to talk about cancer screening. In those who already have had a cancer diagnosis, meaning screening for secondary cancers in cancer survivors, which is a topic that I often get asked about, in my practice. Patients often ask me, [00:01:00] okay, I've had cancer and things are starting to calm down.
my treatment is calming down. My office visits are starting to calm down and I'm starting to regroup about everything, trying to regain control. And one of the things I'm wondering about is I was screening for cancers before my cancer diagnosis Can I get more cancers? And how do we screen for that?
What can I do to reduce that risk? And that is a topic that we're going to talk about today.
[00:01:37] Screening the Survivors: Balancing Vigilance and Value
---
[00:01:37] G van Londen (2): before Colleen and Brad will take a turn, we thought maybe it is, easier, for me to first explain my medical approach to this topic and then let Brad and Colleen respond. So I will first start with my medical spiel that I use to [00:02:00] explain to patients, and that starts by using a visualization almost that I learned from my old mentor, which I find very helpful.
And he used to explain that there are three levels of risk. For the development of cancer, there is the general population to which cancer survivors don't belong anymore because you've had a history of Cancer at this point. On the other end of the spectrum, are those with the, Highest risk of the development of future additional cancers are those with a gene mutation.
Those who carry a gene mutation. The most well-known gene mutations are for the development of, for example, breast cancer, BRCA one and two. [00:03:00] Those carry the highest, lifetime risk of developing cancer. if there is a plus site of these, gene mutations, is that we usually have, a sort of cookbook that will help the providers taking care of these patients.
Screen for these particular cancers and in, many cases even implement treatments that reduce, if not almost completely, negate that cancer development risk. and thirdly cancer survivors without a gene mutation tend to fall anywhere within this spectrum, and that means that the risk of cancer survivors in this category i.e. without a known gene mutation for the development of a future secondary cancer [00:04:00] is truthfully not well-defined.
Many studies are ongoing. But this risk for the future development of secondary cancers in this middle category is highly variable from patient to patient and even from tumor type to tumor type. And that can be highly frustrating because it leaves you with a lot of unknowns. I have to add that there is lots of studies ongoing.
hopefully soon, hopefully within years, we will have more insight into what that risk is and if there is any, targeted slash personalized approach we can do to counsel you more appropriately and hopefully reduce your risk.
But until we have that data, we are often left with recommending cancer survivors without a known gene mutation To [00:05:00] utilize the general population guidelines that are gender and age appropriate in terms of, what to screen for. Sometimes this might be individualized and personalized a little bit depending on, who you are, what your history is, what types of treatments you've been through, because certain cancer treatments, can also increase your risk for cancer Obviously cancer treatments are no fun to undergo. but your doctor prescribed these when you were diagnosed with your first cancer, calculating that your benefits will outweigh the risk. Um, but there might
still be a little bit of long-term risk that, your providers may want to keep an eye on depending on your circumstances. I am not trying to scare you here. If you listen to this overnight, [00:06:00] I'm sure that this doesn't help you fall asleep and or stay asleep, but it's not meant to scare you. Um, it is a, um.
A piece of knowledge that maybe will help you, feel encouraged to discuss this with your providers. The next time, if and when you go and see your doctors, maybe write this down and bring this topic to see how you can improve and or personalize your particular cancer screening regimen.
I know that Brad and Colleen, I see them, writing down all kinds of things. So I'm glad that I will have some supplemental comments, from them. But one more thing to say and I also brought this up in the last episode, but I'm pitching it here again for those who did not listen to the previous episode, [00:07:00] and that is the role for a primary care doctor.
[00:07:03] The Primary Care Provider's Role in Cancer Screening of Cancer Survivors
---
[00:07:03] G van Londen (2): A primary care doctor is one, who can help you with this. If you feel your cancer doctor, doesn't have the bandwidth or the time, to sit down with you and go through this, maybe you can go and discuss this with your primary care doctor, or maybe you can have them communicate together to come up with your personalized cancer screening regimen.
Lastly, before I give it to Colleen and Brad, I wanted to say do not underestimate the power of a screening. It can provide you with a peace of mind, obviously, um, there's two sides to this coin. How long is that peace of mind going to last you? Um, but um, it gives you some sense of control, something you can take care of.
And having said this, I think I'm [00:08:00] going to go to Colleen and Brad and see if they have any additional insights, comments, or if they want me to clarify anything I've said thus far.
[00:08:10] Colleen Dwyer: Brad, Do you wanna go first or do you want me to go first?
[00:08:13] Brad's personal reflections
---
[00:08:13] Brad Buchanan: Well, I just have like my own personal experiences to share, which would certainly go along with, Dr. Josie's, careful, and sensitive reminder that,we don't want to prolong the trauma of an initial cancer diagnosis.
it is possible that some of the treatments we've gotten for our cancers make us more vulnerable if they degrade our immune systems, for example, and that, so this is where I will share my story, that, after my stem cell transplant, I had a very bad case of acute graft versus host disease, and that meant that my immune system, my new immune system, which had replaced my old immune system.
Was kind of going haywire and attacking various parts of my [00:09:00] body and was threatening to kill me. So they had to use a lot of prednisone and other immune suppressant medications to basically, weaken the functioning in my new immune system. And so about six months after my transplant, they did a bunch of blood tests and that's how they found it.
'cause I certainly didn't feel anything. or know anything was wrong, but they did some blood tests and said, well, actually, now you have B-Cell Lymphoma as a consequence of the virus called the Epstein-Barr virus that, a lot of people have, but it doesn't harm them because their immune systems are up to the job of, fending it off, or, preventing it from developing into anything more serious.
I still don't really understand how a virus becomes a cancer, but that's a tale for another day, I suppose. But anyway, um, you know, after my transplant I was going in regularly for blood tests. They weren't worrying [00:10:00] about, my initial cancer coming back necessarily because they saw that I was fully engrafted.
Because my immune system had been so suppressed for such a long time, they really didn't know, what to expect. And so I would go in for blood tests to screen for all kinds of things, to measure my levels of this, that, and the other, chemicals. and it just so happened that on one of those regular blood tests, they caught something of grave concern. I wasn't worrying about getting a second type of cancer to be honest with you. but that was a wake up call and it was, it sort of added, an extra layer of stress and difficulty at a time when I was already very sick. 'cause I certainly had not recovered from my acute graft versus hosts disease fully at all.
I was blind at the time 'cause I had acute ocular graft versus hosts. I had to get myself to a clinical trial in New York to see if they could cure, the second [00:11:00] type of blood cancer that I had, So anyway, without that supplementary screening, that sort of routine, the routine blood tests that they were doing on me regularly, they might not have caught that second lymphoma in a timely fashion, you know, as it happened.
I never experienced any symptoms from that lymphoma. They caught it early enough and they actually treated it successfully here in Sacramento before they treated me at the clinical trial. long story short, that second cancer was a blip on my medical radar.
It was almost kind of like a little funny side trip that my medical journey took into what seemed like, you know, death. But then it turned out to be, oh, no, you're gonna be fine. Back, you go. And, and so I went home from the clinical trial about two months after being given this horrible diagnosis and, went back to recovering from my, graft versus host disease once again.[00:12:00]
But yeah, that was my wake up call to the fact that, you know, my compromised immune system was gonna render me vulnerable to more types of cancer potentially anyway. And that the sooner I could get off all the immune suppressant medications, the healthier I'd be long term. And, you know, I've since had other screenings and, and tests for different types of cancer.
for a long time I was very concerned that the gastrointestinal symptoms I'd had of graft versus host were gonna render me very vulnerable to colon cancer. And so every now and then, well, I think once every couple of years I would go in for these colonoscopies and, the colonoscopies were very frustrating because every single time they would tell me I had prepared poorly and the results were not gonna be helpful.
As it turned out, I take a medication that. discolors my guts and it makes it seem like my prep has been much worse than it [00:13:00] really has. 'cause I was of course, following all my, all the directives, but I take a yellowish medication, right? That means that what comes at the other end is never gonna be nice and clear.
and they told me to keep taking my meds. Of course. Because I think that that's like an antibacterial or an antifungal medication anyway, that I, I kind of depend upon. So anyway, however, I did talk to another doctor, recently, maybe a year and a half ago who said, well, actually, Brad, you're not really at higher risk for colon cancer and these colonoscopies are not helping.
They would catch the odd, like precancerous polyp, but that's about it. and they said, why don't you just use Cologuard and forgive me for using a brand name here? But it has been a bit of a game changer, I think, for a lot of people dealing with, you know, or concerned about colon cancer.
Anyway, instead of getting this kind of punishing and in my case, completely inconclusive, colonoscopy done, every now and then, we poop in a box and mail it off and [00:14:00] it's. And I indeed came back that I had no particular reasons to be concerned. so that's another form of screening that I'm gonna continue to do.
I still do worry that my stomach has been problematic for the last 10 years, I know enough colon cancer patients to know that is a rough go. And I'm not sure I would stand up to all the treatments and the surgeries that they've had to stand up for.
But anyway, tho that's my little, screening for additional cancer narrative for whatever that's worth.
[00:14:30] Colleen Dwyer's Perspective
---
[00:14:30] Colleen Dwyer: Well, I was just gonna add to that, Brad, you know, from doing the Living Life post-cancer treatment program and then of course all of the other. stories that I've heard through the years at Cancer Bridges, from members about the follow up. the anxiety that it can bring on. Again, I know we talked about this a little bit last time too, but, the fear of having to do another set of tests,
All the different emotions that come along with that. Maybe some anger as [00:15:00] well is like, I just don't wanna have to do this stuff because I've been through treatment, particularly around mammograms. I know there's a lot of anxiety about going in for the first mammogram and just what will they find?
Or even colonoscopy, you know, what will they find? and just the fear around that and what that can do to people. Josie, you said earlier, you know, to have this conversation with your, maybe your PCP or your oncologist about these follow up tests. I do think that sometimes that's not an easy conversation to have, or sometimes people don't wanna bring it up because they don't wanna have to do those tests, even though we know it's what we should be doing, and we know it's important, especially if you've had that cancer diagnosis.
It's not always. Top of the list of things that you wanna bring up. So, but it is really important because there are positives to it. If there is something that they can find and they find it earlier, on a prescreening, then that's a good [00:16:00] thing. so, you know, there's reasons to do that.
Plus sometimes people say when they're done with treatment, They aren't being seen as frequently and that it gets a little scary as well, or concerning 'cause there's not a medical person that's putting an eye on them. so sometimes having some of these screenings is a way to, for somebody to be checking in on them and just making sure that, you know, there's not something that's going on that they need to be aware of.
So I was sort of thinking of it more from the social and emotional perspective, I guess, and just what these screenings is, they can be very helpful, but they can also create, again, some of that worry or anxiety, some of those different emotions that can come along with this whole cancer journey.
[00:16:47] Genetic Counseling Referral
---
[00:16:47] G van Londen (2): Yes, thank you Brad and Colleen. while both of you were talking, I suddenly started to remember or think about how [00:17:00] sometimes I was asked, how do I know I have a cancer mutation? When do I need to be referred to cancer genetics? Maybe I thought in this particular episode, maybe I can, talk about it briefly because the topic is immense and it's exploding rapidly with all the new developments.
but in general, your cancer doctors will ask you about your family history and your personal history. at the first time, if not one of the first times they see you. And based on that, they will decide if you need to see a cancer geneticist. they often will decide that and dictate it or note, but they may not necessarily tell you if there's no need for you to see one.
So this thought process that they have may not necessarily be [00:18:00] discussed with you if you don't meet the criteria. however I can understand that it may make you think, well, maybe they forgot. They forgot to think about this. Maybe they forgot to refer me. And so this is another thing for you to write down and ask, Hey, do I need to see a cancer geneticist?
The next time you see your cancer doctor?
[00:18:23] What does genetic counseling entail?
---
[00:18:23] G van Londen (2): a cancer geneticist is a, non-physician who is trained, and keeps their certification up to date with all these new developments about all the new, cancer genetic testing that is out there and all the different mutations and whether they're clinically relevant or not.
This is most often covered by insurance and or your cancer institution
Usually how it works, and I'm talking in general terms. If your [00:19:00] cancer provider thinks you need to see a cancer geneticist, then you make an appointment. There's usually a long waiting time unless they feel your cancer, genetic testing results might determine your active early on treatment plan. Then there is, a way to expedite that.
You would see this geneticist for maybe an hour, and they would draw your whole family tree and calculate your individual risk of carrying a cancer mutation, if that pre-calculated risk of you potentially having a cancer mutation meets certain criteria, then they can send off a cancer genetic testing, after it is approved by the insurance.
It's usually a blood draw. Some cancer mutations need to be drawn or tested at a particular site, and you will get instructions for that. It'll [00:20:00] take about a month for those results to come back. if your results are negative, meaning you have no cancer mutation, then that is it. Nothing really has changed for you.
If there is a cancer mutation, then they will often go through a whole educational path, that will educate you in terms of what it means for you, how can you reduce your risk moving forward. And they will also help you talk with your family in terms of whether they would want to be tested and what it means for them.
there are usually rules and regulations in place for certain insurance policies like, life insurance, to not discriminate against you based on these genetic testing results, but I would ask your genetic counselor when you get to that point, how the [00:21:00] rules and regulations are in the area where you're at.
Last thing to say about this topic, although I can talk forever, is that this is not a one time thing because your family history and your personal history continues to evolve as all of you grow older The medical developments continue to advance. so I usually say if there's a new diagnosis of cancer in yourself or your family member, bring that up the next time you see a cancer doctor and they can see if now you're meeting the criteria of seeing a cancer geneticist. if you, have a cancer geneticist in place already. I would suggest maybe touching base with this person every few years and see if there is anything new that they have learned about your situation.
If you should draw more blood samples, if they've learned anything new about the [00:22:00] previous results so that is my, education on referral to cancer geneticist and what cancer mutations mean.
[00:22:10] Brad Buchanan: Can I ask you a quick question about that Josie?
[00:22:13] G van Londen (2): Yes.
[00:22:15] Genetic Testing is not equally useful yet for all cancer types
---
[00:22:15] Brad Buchanan: Do you know offhand, like what types of cancer are most likely to be predicted by a gene mutation?
[00:22:23] G van Londen (2): Breast, ovarian, colon, pancreatic, and prostate cancers are the ones most often connected to inherited gene mutations — meaning they can sometimes run in families.
[00:22:36] Brad Buchanan: Yeah, no, I just out of interest. Yeah, I was wondering, if it's equally valuable for all types of cancer or mm-hmm. If only a few types of cancer would show up, in such a mutation anyway.
[00:22:53] Colleen Dwyer: definitely seems like there's some cancers that are more related. Like when people share stories, [00:23:00] they'll say, well, my aunt had my second cousin, my, you know, like they'll name off certain people that, like for pancreatic, I think about that. Within the pancreatic group there's a lot of family connection, and then of course breast cancer, prostate cancer.
[00:23:16] G van Londen (2): Yeah. That’s a really good question — genetic testing isn’t equally useful for all cancers. It’s most valuable for certain types, like breast, ovarian, colon, pancreatic, and prostate cancers, because we know specific inherited mutations can increase risk there. For many other cancers, genetics may still play a role, but we don’t yet have clear gene patterns or testing that meaningfully changes care. So the usefulness really depends on the cancer type and family history.
[00:23:50] Ethical Concerns of Cancer Genetic Testing
---
[00:23:50] Brad Buchanan: Now here's another question. it's more of a sort of ethical question, and you already answered one of my ethical concerns regarding genetic testing when you were [00:24:00] talking about, rules in place so that insurance companies don't discriminate against, people who have a certain gene mutation.
Now what about, let's say, I think we've all seen lawsuits, right? Of patients who have, a certain type of lymphoma suing a certain chemical company for reckless, use of a certain weed killing, agent, right? what if genetic testing becomes a kind of get out of jail free card, or how likely is it that genetic testing can be used to discredit patients who are filing lawsuits about, having been made sick by, let's say they were in the military and they were exposed to Agent Orange.
Right. is there a world in which genetic testing would then be, used by these entities that have, polluted or used, cancer [00:25:00] causing chemicals to say, well, you were predisposed anyway because of your genetics, so we're not really responsible for your cancer, despite the fact that there are clinical links between this type of chemical and this type of cancer.
is that a question that's even worth asking at this point?
[00:25:19] G van Londen (2): yeah, it's a complicated question.
[00:25:23] Brad Buchanan: Well, we don't have to spend a bunch of time on it, but I think when you're talking about genetic testing, it opens up a lot of cans of worms, both good and bad,
[00:25:35] G van Londen (2): Yeah, that’s such an important question — and honestly one that worries a lot of people. Like I mentioned earlier, we already have protections such as the Genetic Information Nondiscrimination Act, or GINA, which keeps health insurers and employers from using genetic information against people.
But beyond that, genetic testing should never be used as a free [00:26:00] pass for companies or the military to avoid responsibility for toxic exposures. Just because someone has a gene that might raise their cancer risk doesn’t mean the exposure didn’t play a major role. Most cancers happen from a mix of things — genes, environment, lifestyle — not one single cause.
So even if you have a genetic predisposition, that doesn’t mean you would have developed cancer without that exposure. The key is to use genetic information to protect people and personalize care, not to shift blame or deny accountability
[00:26:38] Family Patterns Without a Known Mutation
---
[00:26:38] Brad Buchanan: yeah, well the topic of blood cancers is of course very near and dear to my heart because, you know, it seems to be running in my family. My grandfather died of leukemia. My mother died of complications of B-cell lymphoma. Which I too have had as well as T-cell lymphoma. And I'm, I have two daughters.
And you know, it would be [00:27:00] nice to know if a blood cancer is unlikely to be genetically, um, carried.
[00:27:05] G van Londen (2): Okay. Let me clarify that. That's a good point. It can cluster in families because maybe you've been exposed to similar environmental exposures because you live in a similar area. Utilize similar water, food, air, who knows?
[00:27:25] Brad Buchanan: Yeah.
[00:27:26] G van Londen (2): Contact. But it could also be, and this is where the medical advancements come to play, that it might be inherited, but we don't know yet for blood cancers what those mutations would be.
[00:27:40] Brad Buchanan: Okay.
[00:27:40] G van Londen (2): and just like for pancreatic cancer where we now know some are inherited, I'm sure at some point, hopefully soon we'll find same for, for blood cancers.
[00:27:51] Brad Buchanan: Yeah. And you've also mentioned certain types of breast cancer have strong genetic, components.
[00:27:59] G van Londen (2): [00:28:00] Yeah, it's amazing to me, like from a pancreatic perspective in the pancreatic group, how many people in that group have family members that have had pancreatic cancer as well?
Yes. And so we are not doing this to scare all of you who sit in their car listening to this or whatever.
We are trying to gently raise awareness and encourage you to not be afraid to ask and talk, so that you can help yourself hopefully live longer.
[00:28:34] Brad Buchanan: Well, you know, there's that old saying, A stitch in time saves nine, and maybe a scan in time also can save nine other scans later. There you go. Showing scarier things. yeah, I certainly know, a lot of guys with prostate cancer, for example, who are, you know, they have their PSA results that they.
Sort of live and die [00:29:00] by, month to month. And as cancer becomes maybe more, in some cases, more of a chronic illness than an acute one, as our means of controlling its bad effects, smarter and less destructive to us. The task of monitoring the cancer becomes even more important. Right. That, that's kind of,
[00:29:25] Benefit Risk ratio for cancer screening
---
[00:29:25] G van Londen (2): you remind me to talk about the benefits and the risks of screening. 'cause we are all assuming here as screening is something you should do, like a knee jerk reflex.
[00:29:35] Brad Buchanan: Right.
[00:29:36] G van Londen (2):
[00:29:36] Brad Buchanan: but it's not,
[00:29:37] G van Londen (2): it's not always the case. for everybody. and so going through the pros and cons, like you described with colonoscopy, it's a big involved prep.
And if the results are minimal, then obviously the benefit risk ratio for you wasn't maybe worth it. and you can make similar benefit and risk ratios in terms of, when to start screening, like for [00:30:00] certain breast cancer, screenings, you may wanna start earlier in age 40. Similarly, when do you stop screening?
As you get older, when you should stop screening. Is there a fixed age or do you do it based on residual life expectancy? And these are all things you can discuss with your cancer providers and your primary care doctor in terms of what are the pros and cons for you, where you are right now in your life
We all have a different philosophy. Some of us are like Tigger and we're bouncing around. We wanna deal with everything proactively. And some are more like Eeyore where we only take care of it if it hits us in the face. And everything is okay as long as you decide for reasons that makes sense to you.
Assuming you have decision making capacity,
[00:30:51] Metavivors and cancer screening
---
[00:30:51] G van Londen (2): One other thing that we were also talking about before we started this podcast is, the fact that there are many cancer survivors [00:31:00] living with metastatic disease and they live for a really long time. because technologies and our treatments have advanced to the point that they can live
some even Decennia. I'm not kidding. in the past that life expectancy was shorter and so we were thinking about maybe screening isn't needed. But if somebody's living with cancer and your life expectancy is deemed to be long enough to benefit from screening, then I would say go for it. Talk with your providers
talk with your providers and see if it makes any sense weighing the benefits and the risks.
[00:31:45] Colleen Dwyer:
I just wanna think about that metastatic piece for just one second. I know you wanna end here, but I do think that's important to say because we don't know who will be listening to this and there are [00:32:00] definitely, like you said, many people that are no evidence of disease, just hunting and trying to figure out how to live and not constantly like to have more of a better quality of life or being somewhat normal. some of these screenings are, it's a normal part of life is, you know, we wanna do these things because you wanna make sure you're doing all that you can to prevent any sort of other issue that comes up.
[00:32:27] G van Londen (2): but it does need to be personalized. Colleen, you brought up a good point because in individuals Who are living with cancer, even if they have no evidence of disease, they often get cancer scans, CT scans and or MRIs. so they may not need to undergo the full panel of cancer screening. Scans usually can't look in your colon. So for, a colonoscopy, that's still something you may have to do or may want to do.
they need a personalized little tweaked screening [00:33:00] regimen, if I make sense.
[00:33:01] Colleen Dwyer: Yeah, and I think it goes back to advocating too for yourself and knowing that maybe you don't have to do all of these, but having open communication with the doctor and talking about like, why would we do this?
Or why is this important and can I rule this one out? Or is it better to actually go ahead and do this for my health.
[00:33:22] Conclusion
---
[00:33:22] G van Londen (2): Yeah, I am very happy Brad and Colleen, that we were able to speak about this topic today. And as usual, I will put links, to the relevant references we spoke about in the, show notes.
if you have any questions, let us know and we will make extra podcast episodes. Catch you the next time.



