CancerSurvivorMD®
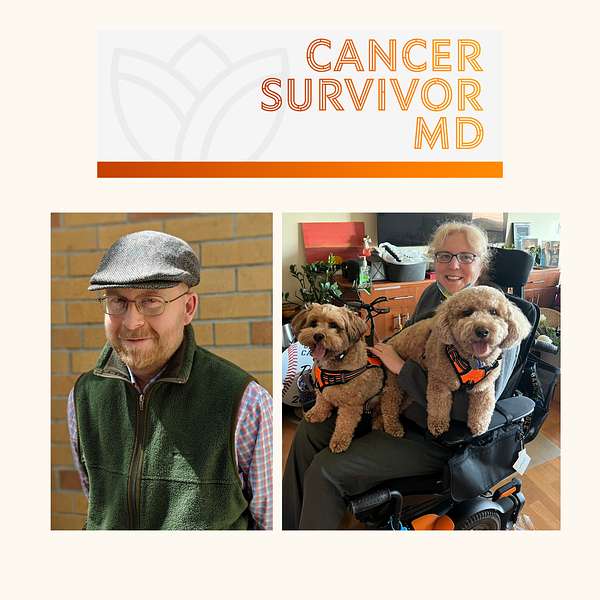
Hello! Welcome to CancerSurvivorMD’s podcast by Brad and Josie!
We will share our experiences with living in sickness, health, and anything in between to allow healing and growth. The topics will focus on cancer survivors and caregivers but will likely resonate with anyone who has been diagnosed with any health condition.
Brad is a retired English professor and cancer survivor, now a facilitator of the Writing as Healing workshop.
Josie is a retired medical oncologist and cancer survivor.
If you have any questions or topic suggestions, please send them our way, and we will try to incorporate your request.
Please take a look at the disclaimers (https://cancersurvivormd.org/disclaimers). Words can hurt—if you feel you might get or have been triggered, please stop listening and seek support.
CancerSurvivorMD®
Survivorchat with Brad and Josie: Cancer Treatment Complications Part 1
Join us as Brad and I dive into the unspoken challenges related to cancer therapies. We share our personal experiences with honesty and vulnerability.
We had so much content that we split it into two parts. This is the first part, in which we tackle the often-overlooked subjects of fertility, intimacy, bone health, accelerated aging, and the emotionally taxing effects of stigmas associated with cancer. In future episodes, we hope to tackle these topics in more detail.
Brad and I share our stories in the hope of resonating with and supporting fellow survivors who are walking a similar path.
General Links:
- Disclaimers: https://cancersurvivormd.org/disclaimers/
- Brad Buchanan: https://linktr.ee/bradthechimera
- G [Josie] van Londen: https://linktr.ee/cancersurvivormd
- CancerBridges: https://cancerbridges.org/
Good morning Brad.
Brad Buchanan:Good morning Josie.
G van Londen:How are you doing this early?
Brad Buchanan:I'm fine, thank you. How about you?
G van Londen:Well, it's almost time for my nap, so after this I'll go to sleep, but I think I have enough energy to do this, and I'm excited because we haven't spoken in a while. I think it's three months ago that we last did this, so it's time months ago that we last did this, so it's time for our next episode. The last episode was the topic of cancer recurrences and the multiple treatments you and I both received, and luckily it was able to get us into remission For both of us. We should knock that off somewhere, but we're very fortunate that we were. However, the treatment came with a cost. Some are short-term side effects, long-term side effects, some are short-lasting, some are long-lasting Side effects often cluster, and today's episode we thought we will talk a little bit about that. We will try to keep it fluffy, but I think many of you can resonate with this, and so we will just see how far we come.
G van Londen:Brad and I decided that I will start, so I will just start talking. So, like I said, I have a whole list here, so I can just list them off and call it a day, but you probably need a little bit more explanation. So one of the things that's made a big impression on me is the fact that after one of my multiple surgeries, which you've heard me talk about in the previous podcast, I developed terrible pain in my belly and it had a sudden onset A few days after surgery. I had a very bad pain in my belly and I'm a little stoic person, so I bit on my teeth and I said I'm sure this will pass, we'll get over it. I didn't have any fever. Do not do what I did. Always contact your doctor if you have an acute belly.
G van Londen:But the next morning I hadn't slept all night and I said to my doctor there's something really wrong. And so I got wheeled into a clinic in the hospital and the minute they put their eyes on me they saw something was wrong. So they fast-tracked me to the hospital room to be admitted, and it took them a few days to figure out what was wrong, which was interesting. I had an ultrasound done first and they said that I massively constipated. There is a large collection of stool in my pelvis and that probably explains the pain. But then I started bleeding like a lot of bleed, and I said I don't, I don't, I don't think this is just stool. And so they went through the communication chain from trainee to attending and eventually it was decided they needed a more advanced scan.
G van Londen:And what they then discovered in that scan is that the collection that they had seen in the ultrasound, that they thought was stool, turned out to be a large collection of bleeding. And, as I've said before, that made me feel very reassured that I'm not making it up, that there is really something happening in my pelvis. It was a very large collection, but by the time they had figured out what it was, the collection of blood had already started to drain itself partially and it had also stopped actively bleeding, because my blood count at that point remained stable. And I can tell you that the pelvis like any part of your body, I guess, where you have a sudden bleeding that needs to take up a large amount of space, that needs to take up a large amount of space that isn't there, is hurting, and so this hurt quite a lot, was quite humbling and I don't know if that explains why for years after that I had a quite painful pelvis. I don't know if the adhesions from the surgery or the scarring from that large blood collection caused the pain.
G van Londen:But, I had to go for many years to physical therapy to try to loosen that up and keep it loose so that I have more range of motion and less pain. I think many of you can recognize yourself in that. Another thing I listed is infections. I got many infections, in particular in my pelvis, in particular in my bladder. Sometimes it was a real infection, sometimes it was false alarm because my bladder is now also a little overactive from the many surgeries and the radiation and they also diagnosed me at some point with radiation cystitis, which is sort of a chronic inflammation state in your bladder that can feel like a bladder infection. So every time I notice something wrong with my bladder, I'm always having a low threshold to bring in my urine sample and have them examine it to see which of these potentially underlying reasons can be explaining my symptoms. An infection in my case with my immunocompromised states, often gets very quickly out of control and drains my whole body. Because of my mitochondrial disease I don't have a lot of reserve, and so that's why I try to catch infections very early. Okay, another thing that I listed here is something that many of us will experience many of us cancer survivors that is, the impact on my fertility. Obviously, the treatments made me infertile. I'm very, very grateful to have one biological child. I realize that many don't even have that opportunity, but regardless, the fact that you've lost your fertility is, on its own, hard to deal with, let alone the impact it has beyond myself. Perhaps, maybe, depending on how things go, we can reserve that topic for another podcast episode. Similarly, with the impact on my sexual life, on my ability to be intimate, as you've heard in previous episodes, due to multiple pelvic surgeries, my ability to have sexual intercourses greatly affected. There are many other ways in which you can be intimate with your partner, which is also something we can discuss in a future episode, but I thought I should at least bring it up here. Next is I became prematurely postmenopausal in my 30s, meaning I am at increased risk for bone loss, for heart disease, hot flashes in particular. For heart disease, hot flashes in particular, if your menopause has an acute, sudden onset, your hot flashes can come on pretty aggressively, pretty intensively, and that intensive aspect of it now has decreased, but I still continue to have hot flashes. In the general population, the rough estimates are that a third of women who continues to have lifelong hot flashes at night spits.
G van Londen:Two more things I listed here. One is constipation. Because of my multiple surgeries and perhaps the radiation my blood vessel and nerve supply, mitochondrial disease my bowels at some point really really moved super, super, super slow, to the point that I'm highly dependent on a bowel regimen to keep me going. As long as I'm sticking to that, I'm fine. I know many of you need to go above and beyond a bowel regimen to keep it going, need to go above and beyond a bowel regimen to keep it going. So in that aspect I think I'm lucky that I just need an over-the-counter bowel regimen, but nevertheless, if I'm not going, it triggers many other things in my pelvis, including my bladder, to act up. Lastly, I wrote down and there's probably more things, but this is what I remembered and I thought I should share with you.
G van Londen:But the last one is stigma. I felt, and I still do, and so talking this way to all of you here required a lot of I wouldn't call it bravery, but stepping over myself to share this information with all of you, because I felt a big stigma for many reasons. One is I felt silly me. I'm a physician and I'm getting cancer and I should know how to first of all, prevent that or manage it, and, second of all, I should know, as a model for my patients, how to emotionally hold myself, and so I felt like I should be a model I should not share, I should not break down. I need to hold myself strong, and my colleagues some of my colleagues were my treating providers, and so that put me in a situation where I also felt like I'm not going to share. And, lastly, my particular cancer was HPV mediated.
G van Londen:As we've discussed before, and I probably will continue to hammer on it, hpv is sort of universal, it's everywhere. There's no need for stigma anymore. The fact that some people develop severe problems from that, like I did, is, for the most part, unexplained, which goes back to the fact that our body is one big black box that we still really don't understand a lot about. But stigma is something that really, really hurt myself in the long run, because I didn't tell individuals, even my family, like my parents, and so it interfered with their ability to help me and my ability to ask for help. Obviously, there's many factors that come into play here, and this topic is multi-layered, but stigma is particularly a topic that has been haunting me for quite a while, and so I think, for now, I'll stop talking and see if Brad has any questions or reflections, because I see his face moving, and so I think he has some things to share. What are you thinking, brad?
Brad Buchanan:Well, I have a couple of thoughts. The first has to do with the stigma that you're talking about, which is, you know, I think, a fascinating topic that doesn't really get discussed anymore, really, that there is still a stigma to some extent about cancer. And, you know, even though cancer is very much now at the forefront of a lot of public discourse, raising awareness about various different kinds of cancer, there's a lot of public campaigns for fundraising and so forth that try to enlist everybody in a sort of collective effort to defeat cancer, beat cancer or what have you. But deep down, I think you know, a lot of us as cancer patients, survivors, however we want to think of ourselves, still have this feeling of you know that now we're somehow and hated in our bodies. That our bodies have produced is really difficult, in a way, to come to terms with.
Brad Buchanan:And maybe your professional identity added an extra layer of stigma that you're the healthy doctor and it's those sick people over there that you're there to help. And then what happens when you become one of those sick people over there? Your profession should have shielded you from that sickness, right? So maybe, in a way, paradoxically, that stigma is even more heightened in your situation. In your situation but because you were, you know, professionally speaking, in a certain relationship to sick people, that that emphasized your difference from them. You know, that's just a. I'm just throwing like possibilities that at you for why that stigma might have been. You know, like personally, like personally, like I've never felt particularly stigmatized by other people for my cancer identity, you know, in a way because I've just sort of accepted it as it's, it's, it's who I've become, and if people can't handle it that's on them. But it sounds like you had a more difficult time accepting yeah, also because, like I said, there's multiple, multiple layers.
G van Londen:One is if, if you're having a chronic health issue, your colleagues know about it and your colleagues have to cover for you, you're becoming a problem person. And you know I'm a. I'm a strong, independent, I can take care of myself person. I grew up on a farm, you take care of your own business, and so I didn't want that label. So that's another reason why I didn't. I kept it to myself. Plus, patients don't don't really, I thought I think, want a provider who is ill themselves and unreliable and not always there, and so that's. However, over time, when I started to take care of cancer survivors, I started to open up more about hey, I had cancer. I didn't tell them which type of cancer. I told them I'm one of you and that helped me create a bond of trust, I think I felt, which was helpful, but I didn't tell them the specific details. I kept that to myself because it's not about me, it's about them.
G van Londen:Now, at this point, now I'm medically retired, I use this particular podcast as one of my outlets to still help, maybe in a different way than I would have if I would have been healthy and I could have continued to see patients in person, but now I'm teaching, empowering, validating individuals through a larger impact on a larger scale, and I feel now I'm ready I don't have to protect myself anymore, I think to share what I've been through, and you are the same at this point.
G van Londen:What do you have to lose? I guess? Yeah, there was very little about my particular situation to read about. There's tons of books about, as you mentioned, breast cancer, colorectal, but there's very little written about gynecology, to be able to read and see what other people have gone through and what to expect. And so the same, I think, with stem cell transplantation. And so I guess I'm describing why we're doing this podcast, but it's just an outlet. At this point, that's doable, is feasible, and my role has evolved, always trying to pivot myself to continue to be able to do things that make me feel like I have a meaning, a purpose, and at this point, stigma is all out of the window, I guess.
Brad Buchanan:Well, that's good to hear, yeah, but yeah, it did sound like. Yeah, you had a very different peer group, let's say, when you were being diagnosed and treated, than I did. And yeah, that there might've been an extra stigma, perhaps in your mind or even in the minds of your colleagues, because you were a woman in what I would assume it would still be a male dominated peer group. You know, doctors yeah, doctors mostly men, mostly men. And also your cancer was of your gynecological area, which I probably don't need to remind you is the locus of a lot of male fear, distrust and othering.
Brad Buchanan:Right that women are radically different kind of creatures because they have this gynecological area which produces life, you know wonderful, but also can make them crazy, like hysterical. That word hysterical is a direct reference to the uterus, a locus of female insanity in the twisted and paranoid male imagination literary reading, let's say of that stigma as well, where you know it plays into a lot of gender issues that might have been at play in your own mind as well, as well as really happening in the way you were treated and viewed by your peers. But let me know if I'm way off track here, but let me know if I'm way off track here.
G van Londen:No, no, like I said, it's multifactorial. There's multiple contributing factors and you're right, that's definitely one of them. Yeah, it shouldn't have to be, but it is. At this point, I think it's important to help future generations to hopefully feel less like they have to hide what's going on with them. Help professionally speaking, because they need the help they can from their colleagues as well as at home. Personally speaking, yes.
Brad Buchanan:Yeah Well, there's probably a reason why there's not as much literature about that type of cancer as there is about other, I don't know less taboo types of cancer. You know that people don't really want to talk about a cancer that affects their reproductive organs as much, you know. It just makes people, makes everyone just a little extra uncomfortable to know oh, you can get cancer there. Yuck, I didn't even know that and now I'm creeped out or frightened or whatever you know. And and just adds another layer of kind of secrecy and taboo to the topic of cancer, which is already uncomfortable. And in past generations their doctors wouldn't even tell them sometimes that they had cancer. But just, oh, there's a terrible disease, you're probably going to die. And they would die of an unnamed illness, a long illness or wasting illness or something like that.
Brad Buchanan:Yeah so we're still in the early generations, at least in the Western world, I would say of like able to speak and name cancer for what it is. Name cancer for what it is, and not just this horrible disease that preys upon our bodies and turns them into monstrous self-consuming, you know, dysfunctional machines.
G van Londen:So that reminds me of one of the earlier author chats we've done, by Dr Elaine Shatner, which is a book that describes the history of how we're talking about cancer. And you're right, it has evolved a lot. Some people are now screaming it of their social media pages that they have cancer and sharing it in extreme detail, but it's a very biased population because not everybody and not every cancer type is sharing this. You're correct.
Brad Buchanan:Yeah, well, I guess another thing that occurred to me as you were speaking. I was listening back to our previous podcasts where we were discussing the fact that my body has kind of been aged prematurely by chemotherapy, just sort of in general, you know my whole work.
Brad Buchanan:I just I feel and maybe look like somewhere between 10 to 20 years older than I really am and it sounds like some of your own biological life has been also kind of accelerated, as you say, to prematurely postmenopausal. Is that the only way that you feel like you've been aged more rapidly by all this, or are there other things that go along with that?
G van Londen:That's an interesting question. How to answer that. That's a huge field that people are really looking into. Cancer treatment is prematurely aging people, and how does that happen? It happens indirectly because it causes us to become prematurely postmenopausal or andropausal for men.
Brad Buchanan:Can you just explain real quick what andropausal means? That's the first time I've ever heard that word.
G van Londen:Oh, it's the male equivalent of a female menopause. Women in average go into menopause. Women in average go into menopause. Their ovaries stop working and they transition to a lower estrogen state, in average at age 51. Men, their testosterone production also decreases, but usually around 10 years later, in their 60s, and so aging can be prematurely accelerated indirectly by affecting these different organ functions. But there's also data that cancer therapies can affect each and every cell directly by affecting its ability for cells to multiply and fix themselves and how long they stay alive. I'm using very generic, simple terms, but I think you get the point that it can cause direct cellular damage. There's many ways that many of the different cancer treatments can affect our aging and we're only beginning to understand that okay, well, thank you for uh explaining.
Brad Buchanan:Yeah, I mean I just never heard that word, but it totally makes sense that men would have an analogous decline in hormone production at that, that age yeah, it's something to keep in mind.
G van Londen:It's hard to measure in men in particular. The official definition of a low testosterone state requires, I believe, you to have it measured a few times to make sure that what you're measuring is accurate. I would, if you have concerns about your testosterone levels or the impact of your treatment on your premature aging state, in terms of your bone health, in terms of your cardiac health, those are all issues that deserve attention. I would write them down for you listeners out there. Just write it down, put it on your list to bring it up the next time you see a doctor and go from there. Hopefully this makes you feel empowered to bring these things up. Yes, it's good that you're still alive, but we want you to live in good health as long as you can, and so you're not complaining by bringing up these items. You're just empowered to take care of yourself.
Brad Buchanan:You're just empowered to take care of yourself. Yeah, I mean I will share that. I had osteopenia at, I think, three years after my transplant, because I'd been taking a lot of prednisone for some time they could tell that my bone density had diminished.
Brad Buchanan:They could tell that my bone density had diminished and so I had to get something called reclassed, which was kind of awful. I felt horrible afterwards and now I take a lot of vitamin D and magnesium oxide and calcium and so forth, and so my osteopenia has apparently reversed a little bit, which is great, because I didn't want to end up with osteoporosis, which would be another way in which my body has kind of aged faster than it otherwise would have done, because of the side effects of the prednisone that they put me on, you know, for good reasons, which I'll get to in a moment. But yeah, that's another sort of aging that my body underwent because of all the treatments and the treatments to rescue me from the treatments, if you get my drift.
G van Londen:Yes, yes, I do, and so that's another thing that maybe we can even do a whole different episode about how to reduce the risk. But, looking at the time, maybe we should now switch over to Brett. Stay tuned for the next episode.

