CancerSurvivorMD®
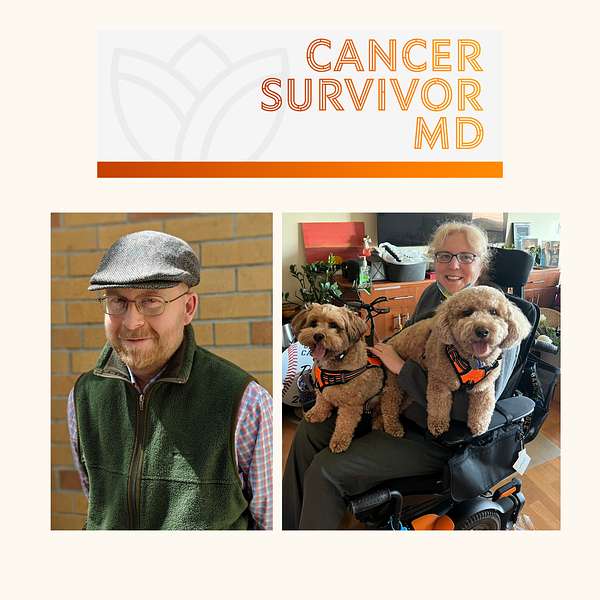
Hello! Welcome to CancerSurvivorMD’s podcast by Brad and Josie!
We will share our experiences with living in sickness, health, and anything in between to allow healing and growth. The topics will focus on cancer survivors and caregivers but will likely resonate with anyone who has been diagnosed with any health condition.
Brad is a retired English professor and cancer survivor, now a facilitator of the Writing as Healing workshop.
Josie is a retired medical oncologist and cancer survivor.
If you have any questions or topic suggestions, please send them our way, and we will try to incorporate your request.
Please take a look at the disclaimers (https://cancersurvivormd.org/disclaimers). Words can hurt—if you feel you might get or have been triggered, please stop listening and seek support.
CancerSurvivorMD®
Survivor Chat with Brad and Josie: Diagnostic Phase of Initial Diagnosis
In this episode, we will be speaking about our personal experiences with the diagnostic part of our journey for our initial diagnosis, such as delay in workup, needing more tissue for diagnostic purposes (multiple times being biopsied, etc.), being a rare case, getting a second opinion, talking with our children, and a bit about feeling gaslighted.
Here are a few helpful links relevant to this episode:
https://www.cancer.org/cancer/caregivers/helping-children-when-a-family-member-has-cancer/dealing-with-treatment/talking-to-kids.html
https://www.cancer.org/cancer/managing-cancer/finding-care/seeking-a-second-opinion.html
General Links:
- Disclaimers: https://cancersurvivormd.org/disclaimers/
- Brad Buchanan: https://linktr.ee/bradthechimera
- G [Josie] van Londen: https://linktr.ee/cancersurvivormd
- CancerBridges: https://cancerbridges.org/
In this episode, we will be speaking about our personal experiences with the diagnostic part of our journey for our initial diagnosis, such as delay in workup, needing more tissue for diagnostic purposes, multiple times being biopsied being a rare case, being biopsied being a rare case, getting a second opinion, talking with our children and a bit about feeling gaslighted. You can find helpful links in the description. Hi Brent, how are you doing today? Hi Josie, not too bad. How about you? I'm happy to be talking with you today. In the last episode we spoke about what brought us here and, naturally speaking, it will be appropriate to talk about the diagnostic journey. My diagnostic journey for my initial diagnosis was very straightforward. My recurrences are a different story, but I think we will reserve that topic for another time, because you and I can fill a whole episode with that. I think maybe for today, let's focus on the initial diagnosis, which brings its own specific dynamics. Brad, if you feel comfortable starting us off, because I think your story for your initial diagnosis was quite a journey.
Brad Buchanan:Yeah, it was a six-month odyssey, basically, of trying to find out what on earth was going on with me. So, just to take you back in time, in the summer of 2014,. Actually, I started noticing like a funny little lump under my jawline. I didn't make much of it. I was also losing a lot of weight. At that time, I had started a new exercise regimen where I was running every day, going to the gym like two or three times a week. So I was in fantastic shape, but I was yeah, I was losing a lot of weight. I went down probably from the high point of about 185 pounds, which was maybe a little too big for a man of my size. I'm about five six, five seven. On a good day I'm 5'7". So I was down to 145 or something like that. But I was just congratulating myself on the success of my fitness regimen.
Brad Buchanan:You know that all that running and lifting weights not big weights, but anyway that that was paying off and I was really in the best shape of my life, I think you could say without a doubt, although later I did find out that one of my colleagues had approached my wife very like, secretly or well, quietly anyway and said Brad's lost a lot of weight. Does he have cancer? And you know my wife at the time, she laughed it off. I said, well, no, of course not. He's just been running a lot and it's kind of annoying how easily he's losing all the weight. You know, just like a man to say, oh fine, I'll lose some weight and do it with no problem. Do it with no problem, anyway. So yeah, the first symptoms that I noticed were basically a lot of weight loss and the funny little lumps under my jaw. But at the end of the summer of 2014, I discovered that the lumps had kind of spread along my jawline. It was more than one and you know, I think I was like huh, this is weird, I wonder what's going on. You know, you know I think I was like huh, this is weird, I wonder what's going on. You know I wear a beard. So, anyway, maybe I thought there was some like follicular problem.
Brad Buchanan:So I went to the doctor. My GP had been kind of in and out of her practice, so I went to see someone I'd never seen before, which was not that unusual, and she sort of went well, I've got no idea, but we'll send you to like a skin specialist because of you know the idea that maybe it was a skin disease or something. So they checked me out. They said, no, it doesn't look like it's anything skin related. I went to an ear, nose and throat specialist after that and they're like no, we don't really have any sense that this is related Like.
Brad Buchanan:I've had a lot of ear infections that turned into sinus infections and so forth in my life so I was wondering if that. Anyway, meanwhile the lumps are spreading. I'm discovering similar inflamed lumps on my abdomen and I'm starting to Google my symptoms at that point and I'm like this doesn't look good. You know, this looks like it might be some kind of cancer. At that point I was like it might be lymphoma, might be leukemia. I really have no idea, but none of the doctors I spoke to would cop to that at all.
G [Josie] van Londen:Wait, brent. So how many months had passed now.
Brad Buchanan:Oh, I, you know. I think we're probably at about the three month mark since I first started noticing the lumps.
G [Josie] van Londen:So initially initially it was my understanding you were like well, do I need to go and see a doctor? But now your emotional state has changed to. But now your emotional state has changed to oh, my goodness, I feel like something is going on here. You're scared. Now I think your emotional state has changed from well, I don't want to be making something out of nothing, but now you're becoming a little anxious, I think.
Brad Buchanan:Yeah, I think that's fair to say, and I also started to in the fall of 2014,. I start to have these just astonishing bouts of night sweats where I would break out in a sweat at night, soak through the sheets on the bed, pretty much completely. I would just drench the bed. So I ended up moving and sleeping downstairs and it got to the point where I was sweating that profusely like two, three, four times a night, which was kind of like to me the clincher, like I have cancer of some kind. I don't know what it is, they don't know, they won't admit that I have cancer, but I was. Also, I went to see an oncologist at Davis Cancer Center and so I had let's see.
Brad Buchanan:I had at least three biopsies. I think One was a fine needle biopsy where they went in with a very small needle and, like, took out a little bit of a lump on my abdomen. They examined it. They didn't find anything of note at that point, so they weren't ready to say, yeah, you have cancer. But yeah, at that point I was pretty fully convinced that I had either leukemia or lymphoma and I knew leukemia could be very deadly. My grandfather died of leukemia and one of my childhood friends died of leukemia when he was just 17, which was a real tragic event in our families and friends' lives, anyway. So finally I got in to see a hematologist at the cancer center who took a bone marrow biopsy. So the big needle stuck into your pelvic bone hurts like hell and he extracted some bone marrow and they did an analysis of that and they said finally yeah, yeah, it looks like you have some type of T-cell lymphoma, but it's rare. We don't know what it's really doing in there. They called it an indolent lymphoma.
Brad Buchanan:It means slow moving and not super threatening. So I was like, okay, all right, I do have lymphoma. My suspicions were justified. I felt kind of vindicated in a weird way. You know, like all those visits to all those different doctors were not just me, you know, wanting attention from the medical community.
Brad Buchanan:I mean, frankly, I've always kind of tried to avoid doctors. I'm very squeamish, I don't like needles, I don't like even giving blood for a blood test is problematic for me. I tend to have to psych myself up. I won't let them poke me in the arm, where most people give blood or get blood tests taken. I want them to poke the back of my hand instead. So anyway, you know I don't really want attention from doctors, but in this case, like, I just felt like yeah, there was something off, something was wrong. So finally getting the diagnosis was a vindication that yes, I do have cancer, but it was. I was basically put in the sort of watch and wait category my initial oncologist because they didn't think that the cancer was going to do much harm to me. They thought it was confined to my skin, basically, or just under the skin. I did ask for a second opinion I wanted to ask you.
G [Josie] van Londen:you were told the cancer is indolent, it's slow growing. But then you had these pretty severe bouts of night sweats and a large degree of weight loss that your wife describes in her book, that she's even concerned that you had an affair.
Brad Buchanan:I forgot that part of her book. That's fascinating, okay.
G [Josie] van Londen:So you lost a lot of weight.
Brad Buchanan:I was having a passionate love affair with cancer, it turned out. Yeah that's interesting.
G [Josie] van Londen:Yeah, but I'm wondering in the back of your mind just to see where you were at that point. Yeah, did you? Did you wonder? You know? Wait a minute, I have all these what we call b symptoms, weight loss and night sweats pretty badly. Is this thing really as indolent as they say it is is? Is that partially what drove you to go and get a second opinion? In hindsight, we always have the benefit of probably. Maybe that's why I did what I did. Yeah, to connect the red dots. But I wonder if, if you, you knew deep down something doesn't jive here well, yeah, there was.
Brad Buchanan:There was definitely part of that. I mean also my oncologist at that time, who did not end up being my oncologist for very long after the diagnosis, but anyway, he said like I'm not a big expert on this type of lymphoma.
G [Josie] van Londen:It's very rare.
Brad Buchanan:Yeah, it's a rare lymphoma. They ended up calling it Brad's lymphoma because it didn't really it didn't fit the normal categories of non-Hodgkin's T-cell lymphoma. It sort of was one of those not otherwise specified types of T-cell lymphoma, but anyway. So yeah, he said like I'm kind of not your guy really. Like he said, well, we could treat it. The only treatment I know that would make any sense is a new treatment called aromadepsin. But it turned out that that was not approved by the insurance company. They wouldn't cover it because it was not approved yet by the FDA as a first-line treatment for cancer. It was only something to be taken after chemotherapy or whatever had failed to deal with the cancer. So he was sort of like I don't know what to do with this. Like it doesn't seem like it's threatening.
Brad Buchanan:But if you want a second opinion and I'd sure, go to Stanford and I'm a Stanford alum, I know that Stanford has a terrific school of medicine and it did seem that they had kind of a cutting edge clinic called the cutaneous lymphoma clinic, which is pretty much what I thought, what everyone thought. I had a lymphoma, just, you know, of the skin area or under the skin. So I went down there for the second opinion and they pretty much concurred with the first opinion, though it's like, well, yeah, we don't think it's super threatening. You could probably go on a hike in the Himalayas, you'll be fine, but we're definitely interested in your case. It's quite an unusual thing you've got going on there. So, yeah, they basically concurred with the first diagnosis that it was not immediately threatening Because the cancers of the skin, you know, unless there's some like really malignant melanoma, the blood cancers on the surface of your body nah, not such a big deal, I gather, and I didn't really feel sick, is the thing.
G [Josie] van Londen:Except for your B symptoms.
Brad Buchanan:Yeah, except for the night sweats, which were just kind of an inconvenience, frankly, and all the weight loss and I did, there was, yeah, there was another symptom I became like pretty easily fatigued. Yeah, like towards the evenings, you know, my wife and I'd be watching a show on netflix and I would I'd be nodding off earlier than I might otherwise do. But yeah, I and I was just curious also like what's going on here and so, yeah, I did want that second opinion and I got it, but it more or less confirmed the first opinion that we don't have any obvious treatment for you yet, because your symptoms are not bad enough really to warrant any interventions and the only thing that we can think of is this drug that you know is not going to get paid for and in fact we're not sure if it's really advisable. I still don't know whether romidepsin would have helped my condition.
Brad Buchanan:I doubt that it would have, frankly, because the cancer, as it turned out, had burrowed into my left lung and there was a tumor that went undetected. Even at my time of diagnosis they didn't understand that the tumor was there. They did some x-rays that showed a slight opacity in my left lung and I was coughing, actually quite a bit Like I was still very physically active. I still ran a ton. I played soccer, you know, twice a week with my usual team. But yeah, I would have these like kind of not great fits of coughing.
G [Josie] van Londen:So it seems like, over the course of a couple of months, your symptoms are progressing and you're developing new symptoms that then progress.
Brad Buchanan:Yeah, yeah, fairly slowly and like the symptoms didn't really connect to an obvious diagnosis for quite some time. And even when they did come up with a diagnosis, it didn't account for the coughing right. So, yeah, so again, this is why I came to be known as a zebra right that the horse breeds they were taught to look for, you know, are the usual ones, the more common diagnoses, which makes sense. I guess it's a version of Occam's razor. You know, like the simplest explanation is usually the most plausible explanation, is usually the right one.
Brad Buchanan:But that was the most common one the usually the right one, but that was not the most common one.
G [Josie] van Londen:Yes, yeah, yeah, but some somebody has to be, somebody has to be in the small percentages yes, and unfortunately uh, or fortunately, I don't know I was in the small percentage.
Brad Buchanan:So I, yeah, I eluded diagnosis for about six months and then, even after my diagnosis, I was in a bit of a limbo, like what do I do? Like they won't approve a medication for me. There was nothing I could do that I knew of, you know, to like slow down the growth of the cancer or try to inhibit it. There was nothing, nothing to be done except sort of watch and wait and hope. Inhibit it. There was nothing to be done except sort of watch and wait and hope that it wasn't something nastier than they thought it was.
G [Josie] van Londen:I can imagine that there's also a lot of waiting for the test results. I read that some of your testing was done right before the holidays the Christmas holidays.
Brad Buchanan:Yeah.
G [Josie] van Londen:And you didn't get the results until after, and so that last Christmas, before your diagnosis, sort of already had a dark cloud hanging over it, because you were waiting for the test results, and that's never easy, the uncertainty of not knowing what will happen, what will be yeah, I, I mean, I remember, you know, talking to my wife and saying you know, I I'm pretty certain I know what these test results are going to say, but it was too early to say anything to the girls at that point.
Brad Buchanan:However, after I was officially diagnosed, we decided we need to tell them, and they were six and 10 years old at the time and it was a really tough decision, like how do we tell them? Do we tell them separately or do we tell them at the same time together? We chose to do it separately Because they were at such different developmental stages. You know, at that age how much they really understand about cancer is was questionable. We just didn't't know. So when we told our 10 year old, she got the emotional gravity of the situation very quickly. She asked quite a few fairly intelligent questions about it. What does this mean? And again, we were still in the watch and wait phase, so we didn't know really what it meant and we kind of said so like yeah, we don't know. But here's, he has a cancer diagnosis. And then she made a plan to tell three of her friends a day to try to keep some control over the situation, which is a very interesting approach. But yeah, I, I knew she was. She was distressed by this. Nora was our 10-year-old and yeah, she's always been sort of a thoughtful, introspective person who is very careful about what she shares with the world. When we told Lucy, our six-year-old, it was a very different reaction. She you could tell, like just by her facial expression, that she was just kind of stunned and didn't know what to do or what to say. Within 10 minutes or so she was dancing around, she had taken off her pants, was kind of acting out, you know. Whatever feelings came up from that information, probably in a way that she wouldn't have done if the 10 year old had been in the room, like modeling a response for her. So I I do wonder whether we would have done better to tell them at the same time. But anyway, that's, that's the way we did things and and each had the response that was authentic to them at that time.
Brad Buchanan:We had to take a couple of steps. As a result, we had to give away our cat, charlie, who was very special, especially to our younger daughter, lucy. She wanted a cat and she wanted to name it Charlie after my first cat that I had adopted when I was a little older than she was, but anyway she wanted to sort of give me back the cat that I had lost when I was young. Charlie died rather tragically. The first Charlie died rather tragically. He was looking out the window on my desk in my room, looking out the window at his nemesis Boris, a neighborhood cat, and had a heart attack and just collapsed and died on the desk.
Brad Buchanan:And yeah, it's a famous family story where I was delivering papers that morning and I came home and my dad told me sorry, charlie's dead, and he showed me Charlie in his little box and I asked did you close Charlie's eyes? Yes, he closed Charlie's eyes. So anyway, I went back out of my paper route to finish delivering and I was crying and was rubbing my eyes with my hands that had, you know, newsprint on them and I came home looking like I you know I had a mascara. It was very hard actually to give charlie away because, you know, the family pet is very important and, um, we just didn't feel like it was a good move to keep charlie around well, you're saying that, I think from the aspect of infection risk, with a cat because you knew your infection risk was going to be high in cats or harbors or all kinds of organisms be around when you're undergoing treatment to suppress your immune system.
G [Josie] van Londen:But this is what Brad's situation was, and that's very sad because the cat was supposed to be a support animal and then, on top of a pretty devastating diagnosis, the one animal that was supposed to give him comfort he had to let go of a second time.
Brad Buchanan:Wow, yeah Well, and also you never know what kids think or believe is going to happen in such a circumstance. You know, and I could tell that Lucy was upset by this whole thing, and I could tell that Lucy was upset by this whole thing. And one time and maybe I was crazy to do this, but one time I sort of took her aside and I said you know, lucy, we did have to get rid of Charlie because I had cancer, but you know that we're not, we're never going to let you go, like we're not going to get rid of you, you know, as another junior member of the family, like you're here to stay no matter what. And then we actually had a nice conversation and during that conversation she asked me to give her a pinky promise that I would live long enough to see her own children and I felt like this was a promise I couldn't afford not to make. I felt like this was a promise I couldn't afford not to make. You're not supposed to make these promises to kids that you don't know that you can fulfill. So maybe it wasn't great parenting, but it was a moment of real emotional bond with her. She could do to try to help me, you know and encourage me is like make me beholden to this promise that I made to her and honestly, like the kids, have been my primary motivation and trying to survive all this stuff.
Brad Buchanan:So their reactions to my diagnosis were really important Moments of kind of inflection in my relationship with them where I think it actually brought us closer emotionally, maybe as parent and child, than we'd ever been before.
Brad Buchanan:I mean, that made it doubly difficult to go into the hospital for my treatments when those treatments became necessary. And it was probably pretty traumatic when they saw my, when I started spitting up blood one fine Saturday evening just before dinner time and I had to rush into the ER after my cancerous tumor burst in my lung, maybe two months or so after I was actually diagnosed. But anyway, the diagnosis, telling the girls about the diagnosis and then their reactions to that, those were really important moments for our family and for my sort of my mission in life was just like just survive, buddy, just survive. Do whatever it takes right, show up to the appointments, do what your doctors tell you. You know it's going to be awful and it was awful, but the girls really need their dad and Lucy asking me to promise not to die was you know. Just yeah, it turned my motivation meter up to 11 out of 10, where it has remained.
G [Josie] van Londen:There's so much I can share about that. I don't think there's a perfect way in talking to your children, and I can tell you that I didn't do it right. Children, um, and I can tell you that I didn't do it right, and so age appropriate disclosure is is the way to go when you are ready to disclose it, because it requires on your end um sort of acceptance that this is what is happening. You need to first have it straight in your head before you can talk with your children, and so I wasn't ready to talk with my son, but our son discovered it because I texted with my husband back and forth, and he became older enough that he would play on my husband's phone every now and then, and so he was able to read some things, and so he was scrolling through our phone, my husband's phone, and found the word cancer.
G [Josie] van Londen:And then he came running towards me and this was in a mall somewhere. We were in the winter, probably just trying to, you know, have children play in a playground in the mall. And he came running towards me somehow and he held me very tightly and said Do you have cancer? And I'm like Okay, where? How did you figure that out? Where did you get that from? And he said Do you have cancer? And I asked again where, how?
G [Josie] van Londen:He said I saw something in Papa's phone, oh my. And so that was a little I'm like okay, what am I supposed to? So stuttering, and I stuttered my way through it, not the adult, responsible way. And so what I did is I told him yes, and then he ran away and we had to follow him, and then we sat down and we talked for a little bit, but I don't remember what we talked about. I just remember that this was not the way I wanted to tell him.
Brad Buchanan:No.
G [Josie] van Londen:How old was he? Oh, my goodness, I don't remember anymore, brad. He must have been younger than 13, but probably older than 8. I don't remember if it was at the time of my invasive cancer diagnosis or during one of the previous incidences. I don't remember. I think I must have dissociated or repressed a lot of my memories, I guess.
Brad Buchanan:That's, frankly, I would say that's every parent's worst nightmare is that their child discovers that there's some you know some important medical information that has been transmitted and concealed from the child. So I, yeah, I commiserate with you on that really tough situation. That must have been very difficult to to get through in that moment.
G [Josie] van Londen:But yeah, but yeah I always wonder do you mess up your children?
Brad Buchanan:yeah, well, I mean at 13, I would say the the child is is formed in terms of his character, I would. I would say, but like lucy being only six, I guess that's when they say the kid's character is formed by the age of six. But yeah, she was still looking for clues about how to take this news. She could not really comprehend cognitively what this really meant. But yeah, I'm sure that for the weeks leading up to our conversations with them, they noticed that there was more tension in the house. For sure, there absolutely was.
Brad Buchanan:And like, yeah, silences or meaningful looks here and there exchanged by the parents that were unexplained and, frankly, that's why we chose to tell them when we did, even though we didn't know, like, how bad my cancer truly was. We thought at that point it was the indolent kind, the slow-moving, not super-threatening kind, but it had impacted the climate of the household immensely long enough that we thought, hey, you know, in case they are aware that there's something new going on here, we'd better tell them now and just get it out in the open and so we can talk about it and ask if they have questions and and and. Then my wife and I did not need to be secretive about it. Or, you know, talking in french, like sometimes when the kids were really little and we did not need to be secretive about it. Or, you know, talking in French, like sometimes when the kids were really little and we wanted to speak to each other in a language that the kids did not understand. We would switch to French, oh yeah.
G [Josie] van Londen:Yeah, you can speak French. That is smart yeah.
Brad Buchanan:I mean, I don't think it fooled the kids for very long, because they started learning French themselves in school and their cousins speak French. So anyway, but yeah it just. It did seem like, you know, we had sort of kept this awful truth to ourselves for long enough that we want, we needed to get it out in the open and share it with the girls. When it became objectively true Like not when I was Googling my symptoms and saying I'm pretty sure I have one of those blood cancers that starts with L, and for me leukemia was by far the most more frightening than lymphoma I didn't even understand, I didn't know. I had a lymphatic system.
Brad Buchanan:Frankly, before I got lymphoma, it just was what the heck? I'd vaguely heard of lymph nodes. I had no idea that they had to do with the blood or anything else going on in the body. I didn't understand any of that stuff. So yeah, I was terrified of leukemia and when I was diagnosed with lymphoma it was almost a relief actually, like, hey, I have a cancer, cancer diagnosis, and it's not as scary as I thought it might be. I mean, I was living in a bit of a fool's paradise because my lymphoma turned out to be very sneaky and, um, you know, quite malignant. Uh, once it had spread to enough parts of my body, but I still don't know when that really when the spread started.
G [Josie] van Londen:Wow, brad, that's a good question. It may be one where you will never get an answer to, and in terms of my decision to try to hide my diagnosis from our son, I think one of the drivers was likely the stigma associated with my cancer situation, and another one is that I thought I guess I was a superwoman, I can hide it. I thought, well, I can somehow work through it, but it but it's really hard to hide your physical and or emotional discomfort with something as major as a cancer diagnosis. Children pick up on things and if you don't tell them then they're going to fill in the blanks. And children often assume blame, so they're thinking the tension is about them, and that is not a healthy situation either.
Brad Buchanan:I was going to ask you do you think your professional capacity as a doctor sort of made you feel like, yes, I can compartmentalize, right, I deal with sickness all the time and other people yes, I can compartmentalize, right, I deal with sickness all the time in other people, so I can put my own sickness in that compartment over there and not bring it home with me. It's like I wouldn't bring home a patient's illness and to talk about that at the table normally. Do you think that played a role in your non-disclosure of the cancer? I'm just being very nosy and speculative here, so you can tell me what you want, but I, I'm just, I'm, I'm curious, I'm genuinely curious I think part of it.
G [Josie] van Londen:Yes, uh, because that's how you're trained in medical school and your whole medical training, residency, fellowship it's all about work first and no matter what's going on in your private life, that's secondary and you just somehow have to figure it out. But you show up to work and you do your thing. Yeah, and everybody knows that. So I'm not, it's not a secret, but that is sort of the mindset. You're stoic, you put on your poker face, you're sort of performing when you're a physician, because you're not supposed to show your own private mess that we all have. Basically, you're here to serve the patient and so you're not supposed to bring your own ballast into the relationship with patients, with your colleagues, you know, because if you're off from work, your outpatients will be canceled and somebody has to cover you Our inpatient service, with the potential that you can't pay them back. So I'm on a roll here because I think obviously you triggered something here. But yeah, that is certainly a mindset. You don't tell show unless you have to, and so that's part of it too.
Brad Buchanan:Yeah, so that's maybe my way of saying. You shouldn't beat yourself up for the way your son found out about your cancer, even though that was certainly not what you would have hoped for or planned by way of a disclosure circumstance, of hope for a planned by way of a disclosure circumstance, but in a way you're maybe conditioned to some extent to, to want to. You know, separate rigidly between work life, which you just lump all illness into that work life, even your own illness gets lumped into that life in some respects yeah and just draw a firm boundary between that and family life, which, yeah, that certainly makes sense.
Brad Buchanan:My training as an academic conditioned me to behave in certain ways, and no doubt your training conditioned you to behave in those ways too, and in some respects it's easier, I would imagine, to have a rigid separation between life and work if you can keep it rigid.
Brad Buchanan:But, evidently you know that's challenging. I think that would be challenging for any doctor at any point for their entire career, let alone if they start to have an illness too. That work life is a whole other discussion. Maybe this is not the right time to launch into. Maybe this is not the right time to launch into but yeah, the interplay between your training as a doctor and then having to transition to some extent to your life as a patient. Are you a good patient?
G [Josie] van Londen:Are you a patient that you, as a doctor, would want to have, or vice versa? Yeah, how much do you trust the system, which is, I think, every patient has issues with that how much do you trust the system and your provider? There was something you said that was very interesting oh, mistakes. I think none of us are perfect and we all make mistakes everywhere. I think the biggest thing is to accept the fact that you're going to be imperfect and the outcome depends on how you correct it. We all have a very great capability of being resilient. It's just being there for each other, like you did with your children, to let them know that there is a soft cushion that they can land on. We're all in this together. The other thing that you said that I thought was very nice is you promised her that you'd be alive to see her children, your children's children, and you know you're feeling guilty because you couldn't really promise that, but at the same time, it is your wish, though it's your intent.
Brad Buchanan:Yeah Well, and failing to keep the promise would be its own punishment, after all. Yes, so you know what's the worst that can happen I die and I die. So but yeah, I mean in my worst moments. I would just remember that I have two kids who still need and want their dad around. Even if I'm thick as all get out, you know, lacking in energy, just a total kind of miserable wretch for days, weeks, months at a time, you know I I'm still there. They can still see that I'm trying my best to make it through the hell that we all went through together so that we could have a relationship again, which we have. So, yeah, they are definitely the biggest reason why I'm delighted to have survived, even though my life is very different than it was before. I'm still their father. They are still my daughters.
Brad Buchanan:And that love, you know, was the continuing connection between us that made it all so much more meaningful to survive, when death would have been much less painful.
G [Josie] van Londen:no doubt, I think we're all winging it. Cancer is a very scary diagnosis. The society has made it a very scary like. The survival for those who have had a heart attack might be the same for those who've had a cancer diagnosis. But somehow a cancer diagnosis has a very scary cloud hanging over it, and that also is multi-determined. One reason is that the cancer can be very invasive and deforming and society has turned, turn it into very traumatizing diagnosis.
G [Josie] van Londen:Even children know. That's why your daughter first thing she makes you promise is you're not going to die. Everybody associates cancer with death, no matter how young you are.
Brad Buchanan:When I was growing up, cancer was just a death sentence, basically, like I never knew anyone who had cancer and survived. That just wasn't a thing right in the 80s, early 80s. So anyway, yeah, and I think sharing my diagnosis with an extended friend group and so forth, you realize just how like dramatic people think that that diagnosis is. And by the time I did share it more broadly, I was very ill. Like I didn't come out officially to everyone like on social media as, hey, I have cancer, until my lung had collapsed.
Brad Buchanan:I was in the hospital struggling to breathe in pretty darn lousy shape and I was kind of fighting for my life already in that point. And so the diagnosis was met with like hey, man, you got to stay strong, like, fight the fight, get through it. There was a lot of that warlike mentality that was important in that moment. There was a solidarity in saying, hey, not only do I have cancer, it's already like kind of wrecked my body in an important way. So I do need that kind of support, you know. And it came. It was very important and gratifying that it did come.
G [Josie] van Londen:Yeah, I like that. You said that, brad. I'm grateful that you had a very supportive environment. That helps a lot to reduce your risk of developing PTSD post-traumatic stress disorder.
Brad Buchanan:But we'll reserve that topic for another time. Okay, sounds good.
G [Josie] van Londen:What do you think, Brad? I think we had a good session today. It's always a pleasure talking with you, Brad.
Brad Buchanan:Yeah, no, this is a really important conversation, and I'm learning things about you and your professional background that offer a whole new perspective on what it means to be a patient. Even the topic of diagnosis alone was pretty rich for us to investigate, so I look forward to more conversations.
G [Josie] van Londen:Thank you, brad, me too, thank you for trusting me with this, and thank you all for listening, thank you. Thank you, brad, big hug.
Brad Buchanan:You too Take care.

